Taking medication with food can reduce side effects like nausea and stomach damage, or prevent dangerous interactions. Learn which drugs need food, which avoid it, and how to get it right every time.
Read more
When you swallow a pill, it doesn’t just disappear—it has to be drug absorption, the process by which a medication enters your bloodstream from its site of administration. Also known as medication uptake, it’s the make-or-break step that decides whether your drug works at all, works too hard, or does nothing at all. If your body can’t absorb it properly, even the most powerful medicine might as well be sugar.
That’s why bioequivalence studies, tests that compare how fast and how much of a drug enters the blood are so important. The FDA uses these studies to approve generic versions of brand-name drugs. They don’t just check if the ingredients match—they check if your body absorbs them the same way. A generic pill might have the same active ingredient, but if it dissolves too slowly or gets blocked by food, it won’t work like the original. That’s the core of the 80/125 rule—a strict threshold that says a generic must deliver between 80% and 125% of the brand’s absorption rate to be considered safe and effective.
And it’s not just about generics. Things like stomach acid, whether you take a pill on an empty stomach, or even your age can change how well a drug gets absorbed. Grapefruit juice? It can block enzymes that break down certain drugs, making them stick around too long and cause side effects. Certain antacids? They can stop antibiotics from being absorbed at all. Even the coating on a pill matters—some are designed to dissolve only in the intestines, not the stomach, to protect the drug or reduce nausea. This is why pharmacokinetics, the science of how your body moves a drug through absorption, distribution, metabolism, and elimination isn’t just for scientists—it’s for anyone who takes medicine regularly.
When drug absorption goes wrong, it’s not just about wasted pills. It’s about treatment failure, unexpected side effects, or even dangerous overdoses. That’s why people with swallowing problems, older adults, or those on multiple meds need to pay close attention—not just to what they take, but how they take it. Crushing a pill might seem like a fix for trouble swallowing, but it can ruin the absorption profile entirely. Some pills are timed-release; break them open and you get a full dose all at once. Others are enteric-coated to avoid stomach irritation—crush those and you risk nausea or damage to your stomach lining.
And here’s the thing: absorption isn’t always the same for everyone. Two people taking the same dose of the same drug might end up with wildly different blood levels. Genetics, gut health, liver function, even the time of day can shift how your body handles medicine. That’s why some people need higher doses, and others feel side effects at normal levels. It’s not about being weak or non-compliant—it’s biology.
What you’ll find below are real stories and clear breakdowns about how drug absorption affects everyday health decisions. From why generic drugs sometimes feel different, to how food interacts with your meds, to why some pills just won’t work no matter how hard you try—these posts cut through the noise. You’ll learn how to spot when absorption is the problem, what to ask your doctor, and how to make sure your medicine actually does what it’s supposed to.

Taking medication with food can reduce side effects like nausea and stomach damage, or prevent dangerous interactions. Learn which drugs need food, which avoid it, and how to get it right every time.
Read more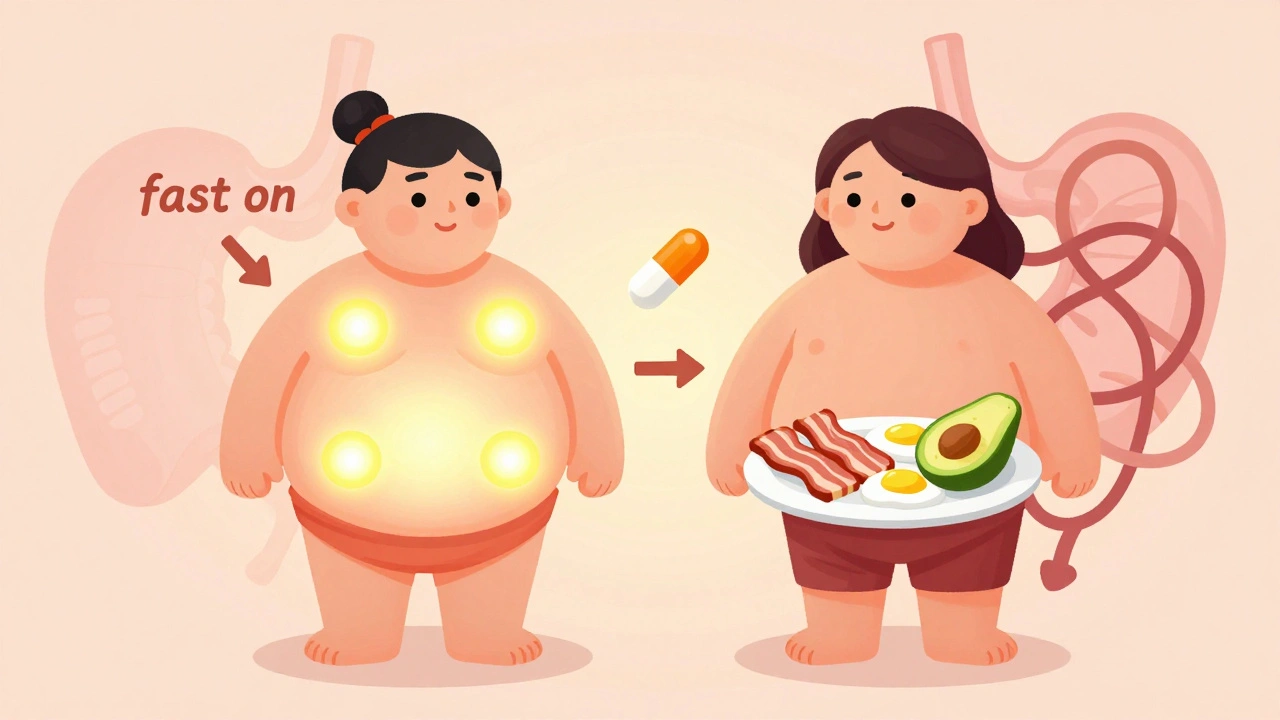
Fasted and fed state testing reveal how food affects drug absorption and exercise performance. Understanding both conditions is critical for safe medication use and effective training. Neither state is universally better-context determines the right choice.
Read more