Compare Esbriet (pirfenidone) with alternatives like Nintedanib, covering efficacy, safety, dosing, cost, and how to choose the best IPF treatment.
Read more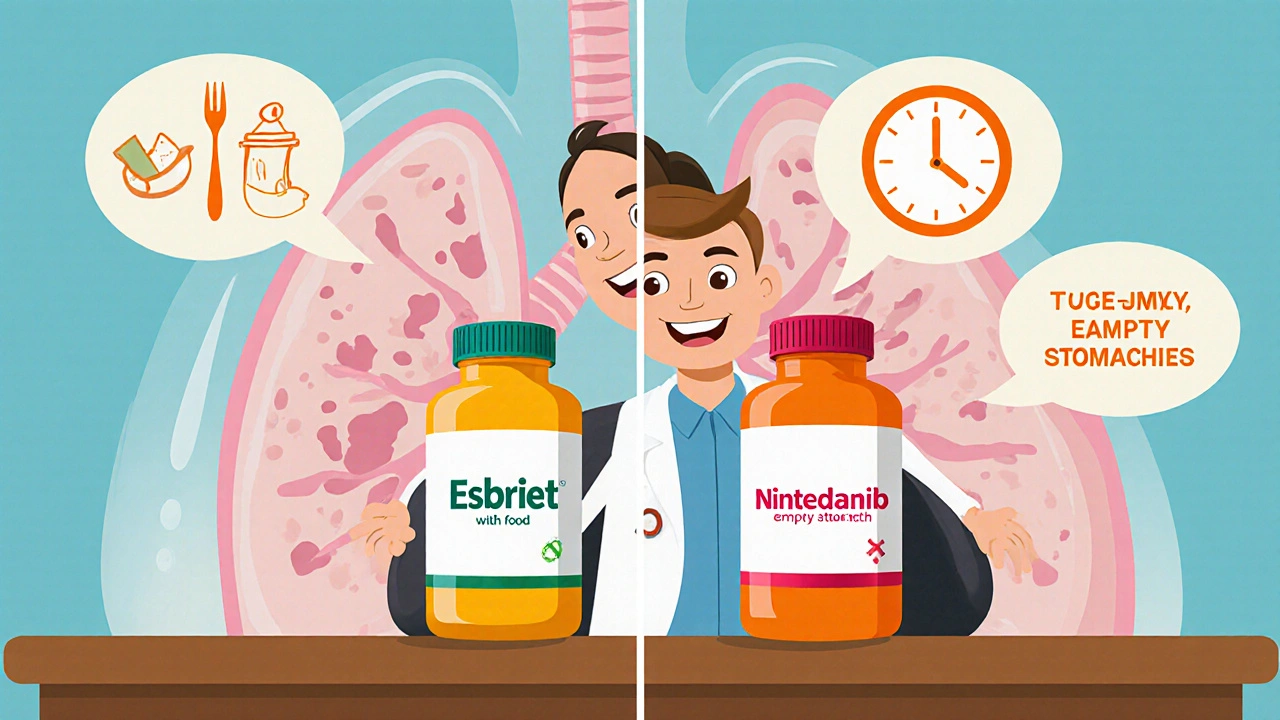
When dealing with IPF treatment, the medical approach aimed at slowing or managing idiopathic pulmonary fibrosis, a progressive lung scarring disease. Also known as idiopathic pulmonary fibrosis therapy, it involves drugs, procedures, and lifestyle support that together try to preserve breathing function.
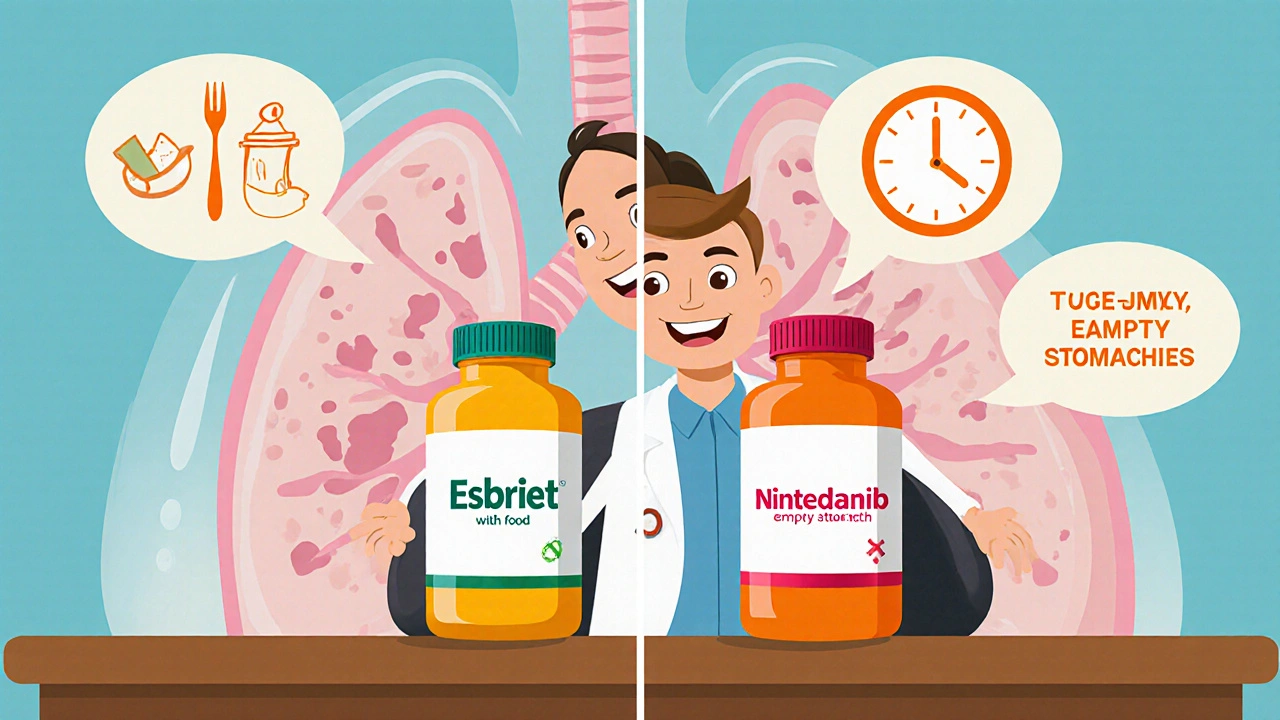
The cornerstone of modern pirfenidone, an oral antifibrotic that reduces collagen buildup and inflammation in the lungs is the first major entity you’ll encounter. It works by inhibiting TGF‑β pathways, which are key drivers of fibrosis. nintedanib, a tyrosine‑kinase inhibitor that targets multiple growth factor receptors involved in scar formation forms the second pillar. Both drugs share the goal of slowing disease progression, but they differ in side‑effect profiles—pirfenidone often causes rash and GI upset, while nintedanib may trigger diarrhea.
For patients whose lung function keeps dropping despite medication, lung transplant, surgical replacement of diseased lungs with donor organs becomes a life‑saving option. Eligibility hinges on age, overall health, and the absence of other organ failures. Post‑transplant care includes immunosuppression, infection monitoring, and rehab to regain breathing efficiency.
Beyond drugs and surgery, pulmonary rehabilitation plays a crucial supporting role. Structured exercise, breathing techniques, and education help patients maintain stamina and improve quality of life. Studies show rehab can reduce hospitalizations and boost oxygen saturation during daily activities.
Clinical trials continue to push the envelope. New agents targeting fibroblast activation, such as lysyl oxidase‑like 2 inhibitors, are in phase II studies. Gene‑editing approaches aim to correct mutations linked to familial forms of IPF, while stem‑cell infusions explore tissue repair potential. Each trial contributes data that refines guidelines and expands the therapeutic toolkit.
Diagnostic precision matters, too. High‑resolution CT scanning (HRCT) provides the imaging backbone for identifying usual interstitial pneumonia patterns, which guide treatment decisions. Biomarkers like serum KL‑6 or surfactant protein D are being validated to forecast disease speed and response to therapy.
Insurance coverage and cost are real hurdles. Many patients compare generic vs brand pricing for pirfenidone and nintedanib, often turning to reputable online pharmacies for savings. Understanding formularies, co‑pay assistance programs, and regional pricing can make a pricey regimen more manageable.
Smoking cessation, vaccination against flu and pneumococcus, and managing comorbidities such as gastroesophageal reflux are non‑pharmacologic strategies that complement primary treatments. They lower the risk of acute exacerbations, which are sudden, often fatal declines in lung function.
In practice, a multidisciplinary team—pulmonologist, pharmacist, transplant surgeon, physiotherapist, and nutritionist—coordinates care. This collaborative model reflects the semantic triple: IPF treatment encompasses antifibrotic medication, transplant surgery, and rehabilitation. It also illustrates that effective therapy requires both pharmacologic and non‑pharmacologic interventions, and that clinical trials influence future standard of care.
Below you’ll find a curated list of articles that dive deeper into each of these areas: drug comparisons, transplant eligibility checklists, rehab program tips, and the latest trial updates. Use the resources to shape a personalized plan, stay informed about emerging options, and connect with experts who can guide you through each step of the journey.
Compare Esbriet (pirfenidone) with alternatives like Nintedanib, covering efficacy, safety, dosing, cost, and how to choose the best IPF treatment.
Read more