Warfarin Dosing Calculator
Personalized Warfarin Dosing Calculator
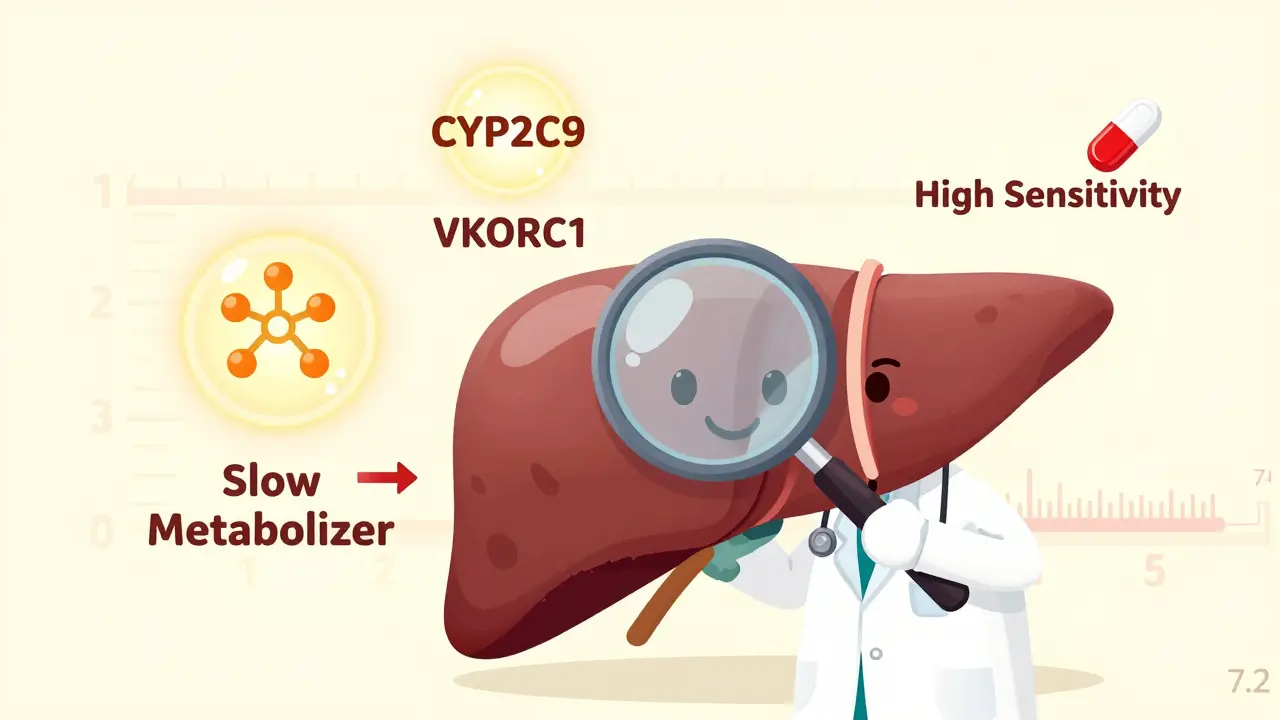
Based on your CYP2C9 and VKORC1 genotypes, we'll calculate your recommended starting dose to minimize bleeding risk.
Recommended Starting Dose
Why This Matters
Genetic testing for CYP2C9 and VKORC1 can reduce your bleeding risk by up to 32%. Patients with high-risk genotypes (like CYP2C9 *3/*3 or VKORC1 AA) often need doses less than half of standard recommendations.
When you’re on warfarin, even a small change in dose can send your INR soaring-or crash it too low. One day you’re stable, the next you’re in the ER with an INR of 7.2, bleeding from your gums. For many, this isn’t bad luck. It’s genetics.
Why Warfarin Is So Tricky
Warfarin has been around since the 1950s. It works by blocking VKORC1, the enzyme your body needs to recycle vitamin K and make clotting factors. Without enough active vitamin K, your blood thins. Simple, right? Not quite.
Warfarin’s narrow window between too little and too much means your dose has to be just right. Too high? Risk of bleeding. Too low? Risk of stroke or clot. In real-world use, most people spend only about 60% of their time in the therapeutic range. That’s why so many end up in the hospital-often because their dose was based on guesswork, not their biology.
The Two Genes That Control Your Warfarin Dose
Two genes hold the keys to why some people need 2 mg a day and others need 10 mg. They’re CYP2C9 and VKORC1.
CYP2C9 is your liver’s main tool for breaking down the powerful S-enantiomer of warfarin-the one that does most of the work. If you have a variant like CYP2C9*2 or *3, your liver slows down. Much slower. Carriers of CYP2C9*3 clear S-warfarin up to 80% slower than people with the normal version. That means the drug builds up. Even a standard dose can become toxic.
VKORC1 is the actual target of warfarin. If your version of this gene has the -1639A variant (especially the AA genotype), your body makes less of the enzyme. That means warfarin doesn’t have to work as hard to block it. You’re naturally more sensitive. People with the AA genotype often need less than half the dose of someone with the GG version.
Together, these two genes explain nearly half of why warfarin doses vary so wildly between people. A 2009 study from the International Warfarin Pharmacogenetics Consortium found that adding CYP2C9 and VKORC1 data to age, weight, and drug interactions boosted dose prediction accuracy from 32% to over 52%.
What Your Genotype Means for Your Dose
Here’s what the numbers look like in practice:
- Someone with VKORC1 GG and CYP2C9 *1/*1 (normal): likely needs 5-7 mg/day.
- Someone with VKORC1 AA and CYP2C9 *1/*3: may need only 2-3 mg/day.
- Someone with VKORC1 AA and CYP2C9 *3/*3: could need as little as 1 mg/day-sometimes less than half a tablet.
That’s not a typo. A person with both high-risk variants can be dangerously over-dosed if started on the standard 5 mg daily. In fact, a 2020 review found these patients had an 83% higher risk of supratherapeutic INR in the first week alone.
One Reddit user, u/WarfarinWarrior, shared their story: after genetic testing revealed they had the CYP2C9*3 variant, their dose was cut from 5 mg to 2.5 mg. Their INR, which had been bouncing between 2 and 6 for months, finally stabilized. Another user, u/ClottingConfused, wasn’t tested. Started on 5 mg. Two weeks later, INR hit 6.2. They ended up in the ER.

The Real Cost of Not Testing
It’s not just about convenience. Not testing can cost lives.
A 2013 randomized trial called EU-PACT showed that patients whose doses were guided by genetics had a 32% lower risk of major bleeding in the first 90 days. Another 2025 meta-analysis confirmed a 27% reduction in major bleeding with genotype-guided dosing.
And it’s not just bleeding. Patients with CYP2C9 variants are nearly twice as likely to have an INR above 4 in the first three months. That’s when most serious bleeds happen. A 2018 study found 18.7% of variant carriers needed medical attention for bleeding compared to 9.3% of non-carriers.
Meanwhile, the average person on warfarin spends more than a third of their time outside the safe range. That’s 120+ days a year at risk. Genetic testing doesn’t just make dosing easier-it makes it safer.
Why Isn’t Everyone Getting Tested?
Here’s the catch: even though guidelines from CPIC and the FDA have recommended genetic testing since 2010, only 5-15% of U.S. patients get tested before starting warfarin. Why?
- Cost: Testing runs $250-$500 out-of-pocket. Medicare covers it under CPT codes 81225 and 81227, but many private insurers don’t.
- Turnaround time: Results take 3-5 business days. Doctors don’t want to delay therapy.
- Knowledge gap: A 2023 survey found only 38% of primary care doctors could correctly explain how CYP2C9*3 affects warfarin metabolism.
- Debate in the field: Some experts argue the number needed to genotype to prevent one major bleed is 200-too high to justify routine use. But that math ignores the cumulative risk for patients on warfarin for years.
Meanwhile, hospitals like Vanderbilt have proven it works. After implementing genotype-guided dosing, patients reached therapeutic INR 1.8 days faster. Fewer visits. Fewer emergencies.

Warfarin vs. DOACs: Is Genetics Still Relevant?
Direct oral anticoagulants (DOACs) like apixaban and rivaroxaban have taken over for many patients-especially those with atrial fibrillation. Why? No monitoring. Fewer food interactions. More predictable dosing.
But warfarin hasn’t disappeared. It’s still the only option for people with mechanical heart valves. It’s still used when kidney function is poor. And it’s still the only anticoagulant you can reverse quickly with vitamin K or fresh frozen plasma.
For these patients, getting the dose right matters more than ever. If you’re on warfarin for life, your risk of bleeding keeps climbing. A 2025 study in Nature Reviews Cardiology predicts that by 2030, 60% of new warfarin users will be tested genetically-because the cost of testing is falling below $100, and the evidence keeps piling up.
What You Can Do Now
If you’re on warfarin-or about to start-here’s what you can do:
- Ask your doctor if genetic testing is right for you. Especially if you’ve had unstable INRs, bleeding episodes, or if you’re on long-term therapy.
- If your insurance won’t cover it, ask about cash-pay options. Some labs offer testing for under $200.
- Keep your INR logs. If your dose keeps changing, it’s a red flag your genetics might be involved.
- Share your results with your pharmacist. They can help flag drug interactions that could push your levels too high.
There’s no magic pill here. But knowing your genes can turn a dangerous guessing game into a controlled, predictable treatment. It’s not about whether you need warfarin. It’s about whether you’re getting the right dose.
What’s Next?
The Warfarin Genotype Implementation Network (WaGIN), launched in early 2025, is tracking 50,000 patients across 200 clinics to prove that widespread testing saves money and lives. Early results from the 2023 REAL-Gene trial already show an 8.2% improvement in time within therapeutic range.
And with the American Society of Hematology expected to update its guidelines in mid-2025, the tide is turning. The question isn’t whether pharmacogenetics works for warfarin. It’s how soon it will become standard.
Can genetic testing prevent warfarin bleeding?
Yes. Multiple studies, including the EU-PACT trial and a 2025 meta-analysis, show that starting warfarin based on CYP2C9 and VKORC1 genetics reduces major bleeding by 27-32% in the first 90 days. This is especially true for people with slow-metabolizing CYP2C9 variants or low-expression VKORC1 genotypes, who are at highest risk of overdose.
How much does warfarin genetic testing cost?
In the U.S., testing typically costs between $250 and $500 out-of-pocket. Medicare covers it under CPT codes 81225 (CYP2C9) and 81227 (VKORC1). Some labs offer cash discounts under $200. Insurance coverage varies widely-many private plans still deny it, despite FDA and CPIC guidelines recommending it.
Do I need genetic testing if I’m on a DOAC?
No. DOACs like apixaban, rivaroxaban, and dabigatran don’t rely on CYP2C9 or VKORC1 for metabolism or action. Their dosing is much more predictable and doesn’t require routine monitoring or genetic testing. Testing is only relevant if you’re on warfarin or considering switching back to it.
How long does it take to get genetic test results for warfarin?
Standard turnaround time is 3 to 5 business days. Some labs offer expedited results in 24-48 hours for an extra fee. This delay can be a barrier in urgent cases, but for planned therapy-like after a stroke or valve replacement-it’s manageable and often worth the wait.
Can I get tested after already starting warfarin?
Yes. Even if you’ve been on warfarin for months or years, genetic testing can explain why your dose has been so hard to stabilize. Many patients discover they’ve been over- or under-dosed for years. A single test can lead to a safer, more stable dose going forward-even if you’ve already been on the drug for a long time.
What if my doctor says genetic testing isn’t necessary?
Ask for the reasoning. If they say it’s too expensive or not proven, point to the CPIC guidelines (2022) and the EU-PACT and REAL-Gene trials showing clear benefit. You can also ask for a referral to a clinical pharmacist or anticoagulation clinic-they’re more familiar with pharmacogenetics. Your safety matters more than convenience.

Shanahan Crowell
Wow, this is the kind of post that makes me want to scream at every doctor who still prescribes warfarin like it's 1998! I had a cousin who bled out from a 5mg dose because no one tested her-she had the *3/*3 combo and they just shrugged and said 'everyone's different.' No, not everyone's different-some people are genetically set up to die from standard care.
Genetics isn't magic, it's math. And math doesn't lie. If your liver can't break down warfarin fast enough, giving you more is like pouring gasoline on a fire. I'm so tired of 'trial and error' being called 'medicine.' It's just negligence with a stethoscope.
Kerry Howarth
EU-PACT data is solid. 32% fewer bleeds. That’s not marginal. That’s life-saving.
Tiffany Channell
Let’s be real-this whole pharmacogenetics thing is just Big Pharma’s way of selling more tests. The real problem is that doctors don’t monitor INRs closely enough. If you’re on warfarin and your INR isn’t checked weekly for the first month, you’re being neglected. Not genetics. Negligence.
And don’t get me started on ‘cash-pay under $200.’ That’s still 200 bucks most people don’t have. This isn’t progress. It’s exclusion disguised as innovation.
Joy F
Think about it: we live in an age where your phone knows your mood from typing patterns, your fridge orders milk before you run out, and your Fitbit predicts your sleep quality-but we still let a 70-year-old GP eyeball your warfarin dose like it’s a fortune cookie?!
CYP2C9*3 isn’t just a SNP-it’s a silent scream from your DNA saying, ‘I’m not built for this.’ And VKORC1 AA? That’s your body whispering, ‘Please, just give me half.’
We’ve mapped the human genome, cracked quantum encryption, and sent robots to Mars… but we still treat anticoagulation like a game of Russian roulette with lab results? We’ve got the tools. We’ve got the data. We just don’t have the collective will to stop pretending medicine is an art form when it’s clearly a science that’s been handcuffed by bureaucracy.
The real tragedy isn’t the bleeding. It’s that we knew how to prevent it for 15 years-and chose convenience over care.
Haley Parizo
You think this is about genetics? No. This is about power. The pharmaceutical industry doesn’t want you to know your genes because then you’d stop trusting them. Why pay $100 for a test when you can pay $300 a month for INR checks, ER visits, and blood transfusions? The system profits from chaos. Genotyping disrupts that.
And let’s not pretend DOACs are the answer-they’re just more expensive, irreversible, and unmonitored. What happens when you’re bleeding and your doctor has no way to reverse it? Vitamin K works. FFP works. But only if you’re on warfarin. So we’re throwing out the only reversible option because we’re too lazy to do the work?
This isn’t science. It’s capitalism with a white coat.
Ian Detrick
I’ve been on warfarin for 8 years. My INR used to swing like a pendulum-2.1 one week, 6.5 the next. Then I got tested. CYP2C9*1/*3. VKORC1 GA. They dropped me from 6mg to 3.5mg. Stable ever since. No more ER trips. No more anxiety every time I get a cold or start a new antibiotic.
It’s not complicated. If your dose keeps changing, your genes are talking. Listen.
Angela Fisher
Did you know the FDA knew about this in 2010? And yet they didn’t force labs to make it cheap. And the doctors? They’re all trained in the 90s. They don’t even know what CYP means. I think this is all part of the government’s plan to make us sick so they can sell us more meds. They want us dependent. That’s why they won’t cover testing. It’s not about cost-it’s about control.
And don’t tell me about ‘evidence.’ The same people who said smoking was safe said this was ‘not cost-effective.’ Look where that got us.
My cousin’s dad died of a brain bleed after 3 weeks on warfarin. He was 62. No test. No warning. Just a ‘standard dose.’ I swear to god, if I ever need warfarin, I’m flying to India to get tested. At least they’re not lying there.
Neela Sharma
My uncle in Mumbai was on warfarin for atrial fibrillation. No testing. Dose kept changing. He got dizzy, fell, cracked his skull. Turned out he had the AA genotype. They finally tested him after the fall. Dose halved. He’s fine now.
Here in India, we don’t have fancy labs everywhere-but we have common sense. If your blood won’t clot right, look inside the body, not just at the numbers.
Genes don’t care about insurance. They just are.
Shruti Badhwar
While the clinical evidence supporting pharmacogenetic-guided warfarin dosing is robust, the implementation gap persists due to systemic barriers including physician education, reimbursement policies, and logistical constraints related to test turnaround time. A multidisciplinary approach involving clinical pharmacists, electronic health record integration, and decision support tools is imperative to bridge this gap. Without structural change, individual patient advocacy remains insufficient.
Brittany Wallace
I just want to say thank you for writing this. I spent years thinking I was broken because my INR never stayed right. Turns out I was just genetically unlucky. Getting tested felt like finally being seen. I’m not a bad patient. I just needed the right key.
To anyone reading this who’s struggling with warfarin: you’re not failing. The system is. But you can still fight for your life. Ask for the test. Bring this post to your doctor. You deserve to be safe.
Michael Burgess
Biggest myth: 'DOACs are better.' Nah. They’re easier for docs, but worse for patients who need reversibility. My dad had a mechanical mitral valve. DOACs? No go. Warfarin was his only shot. They started him at 5mg. He bled into his gut. Took 3 units of blood. Then they tested him. CYP2C9*2/*3. VKORC1 AA. Dropped to 1.5mg. He’s been stable for 4 years now.
Don’t let anyone tell you genetics is 'too niche.' For the people who need it? It’s everything.
Liam Tanner
My mom’s on warfarin. She’s 78. We got her tested last year. Turns out she’s CYP2C9*1/*3 and VKORC1 GA. Dose was 7mg. Now it’s 3.25mg. She hasn’t had a single INR panic since. I just wish we’d done this 5 years ago.
It’s not expensive. It’s not hard. It’s just not prioritized.
Palesa Makuru
Okay but have you considered that maybe people just don’t care enough? Like, sure, genetics matters-but do you really think the average person is going to go get tested when they’re already overwhelmed by 10 meds, 3 doctors, and a $500 deductible? This isn’t a science problem. It’s a human problem. And humans? We’re lazy. We wait until we’re bleeding out before we ask questions.
So yeah, test everyone. But also-teach them. Before they start. Not after the ER.