Penicillin Allergy Risk Assessment Tool
Assess Your Reaction
Results & Recommendations
Enter your information above to see your personalized risk assessment.
What You Should Do Next
After completing the assessment, you'll see your personalized next steps.
More than 10% of people in the U.S. say they’re allergic to penicillin. But here’s the surprising truth: penicillin allergy is often misdiagnosed. In fact, fewer than 1% of those people actually have a true immune system reaction. The rest? They’re confusing side effects with allergies. And that mistake isn’t just inconvenient-it’s dangerous.
What’s the Real Difference Between an Allergy and a Side Effect?
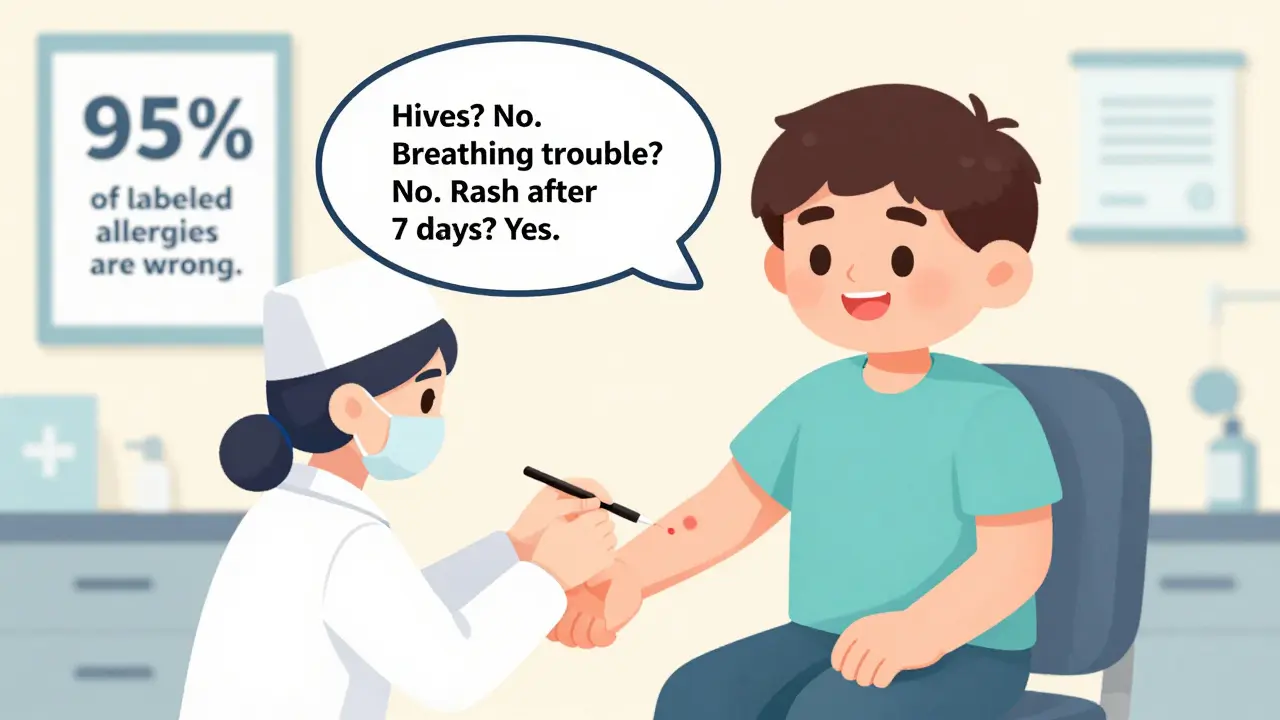
An allergic reaction to penicillin means your immune system sees the drug as a threat. It kicks into high gear, releasing chemicals like histamine that cause symptoms ranging from hives to life-threatening anaphylaxis. This is rare-and it’s not something you grow out of overnight. True penicillin allergies are IgE-mediated, meaning they happen fast: within minutes to an hour after taking the drug. Side effects? Those are completely different. They’re not your immune system reacting. They’re just the drug doing things your body wasn’t designed to handle. Think nausea, diarrhea, or a mild rash. These are common, usually harmless, and go away when you stop the medicine. But because they show up around the same time as an infection, people often assume they’re allergic. Here’s a real example: A child gets amoxicillin for an ear infection. A few days later, a red, blotchy rash appears. The parents panic. The doctor says, “You’re allergic to penicillin.” But that rash? It’s often caused by a virus like Epstein-Barr-not the antibiotic. Still, that label sticks for life.Why Mislabeling Penicillin Allergies Is a Public Health Problem
When someone is labeled allergic to penicillin, doctors avoid it. That sounds safe-but it’s not. Instead, they reach for broader-spectrum antibiotics like vancomycin, clindamycin, or fluoroquinolones. These drugs aren’t just more expensive. They’re more dangerous. Studies show people with fake penicillin allergy labels are 45% more likely to get a Clostridioides difficile infection, a severe gut infection that can land you in the hospital for weeks. They’re also more likely to develop MRSA, a tough antibiotic-resistant staph infection. One 2019 study found that patients with mislabeled penicillin allergies had 6 more deaths per 1,000 within a year of hospitalization than those who could safely take penicillin. The financial cost is just as bad. Hospitals spend an extra $1,000 per admission when they can’t use penicillin. That’s because alternatives cost more, require longer stays, and often need extra monitoring. In the U.S. alone, this mislabeling contributes to $20 billion in unnecessary healthcare costs every year.What Does a True Penicillin Allergy Look Like?
True penicillin allergies have clear signs. They come on fast and involve your immune system:- Hives (raised, itchy red welts)
- Swelling of the lips, tongue, or throat (angioedema)
- Wheezing or trouble breathing
- Dropping blood pressure (leading to dizziness or fainting)
- Anaphylaxis-a full-body reaction that can be fatal without immediate epinephrine
Side Effects That Are Common (and Not Allergies)
Most people who think they’re allergic to penicillin actually just had one of these common side effects:- Mild nausea or upset stomach (affects 5-10% of users)
- Diarrhea (1-2% of users)
- Vaginal yeast infection (due to disruption of normal bacteria)
- Headache or dizziness
- A mild, non-itchy rash that fades on its own
How to Find Out If You’re Really Allergic
If you’ve been told you’re allergic to penicillin but never had a severe reaction, you might be able to get that label removed. Here’s how:- Talk to your doctor. Ask if you can be referred to an allergist. Don’t wait until you’re sick-do it during a routine visit.
- Get a skin test. This is the gold standard. A tiny amount of penicillin is placed under your skin. If you’re truly allergic, a red bump will form within 15-20 minutes.
- Take an oral challenge. If the skin test is negative, you’ll be given a small dose of amoxicillin under supervision. You’ll be watched for an hour. If nothing happens? You’re not allergic.
Why Most People Can Safely Take Penicillin Again
Here’s the best part: even if you had a real allergy years ago, you might not have it anymore. Penicillin-specific IgE antibodies fade over time. After 10 years, 80% of people lose their sensitivity. That means if you were told you were allergic as a kid-especially if the reaction was just a rash-you’re probably fine now. A 2010 study showed that most people who avoided penicillin for decades could take it safely after testing. The key is testing. Don’t assume. Don’t guess. Get checked.
What’s Changing in Healthcare
Hospitals and clinics are waking up. In 2018, only 22% of U.S. academic medical centers had formal penicillin de-labeling programs. By 2023, that number jumped to 68%. Why? Because it saves lives and money. Pharmacists are now leading these programs. At Kaiser Permanente, pharmacists evaluate 15-20 patients a week. They use simple tools like the PEN-FAST score to quickly identify low-risk patients. Those patients skip skin testing and go straight to an oral challenge. New tech is helping too. The CDC and University of Pennsylvania developed a smartphone app called PAAT (Penicillin Allergy Assessment Tool). It asks you five simple questions and tells you your risk level. It’s 94% accurate at spotting who needs testing. Starting in 2025, Medicare will start rewarding hospitals that reduce unnecessary antibiotic use-including by removing false penicillin allergy labels. That means this won’t be optional much longer.What You Can Do Today
If you’ve been told you’re allergic to penicillin:- Don’t panic. Most people aren’t truly allergic.
- Look back at your reaction. Did it happen within an hour? Did you have swelling, breathing trouble, or low blood pressure? If not, it’s likely a side effect.
- Ask your doctor for a referral to an allergist. Say: “I think I might have been mislabeled. Can we test me?”
- Bring your full history. What symptoms did you have? When? How long did they last? Were you treated with antihistamines or epinephrine?
Final Thought: Your Label Doesn’t Define You
A penicillin allergy label is just a note in a chart. It’s not a life sentence. And it’s not always accurate. Millions of people live with a label they don’t need. That label keeps them from the best treatment, increases their risk of dangerous infections, and costs the system billions. You don’t have to live with it. You just need to ask the right question: “Could this have been a side effect-and not an allergy?”Can you outgrow a penicillin allergy?
Yes. Studies show that 80% of people who had a true penicillin allergy as a child lose their sensitivity after 10 years. Even if you had a severe reaction in the past, you may still be able to take penicillin safely today. The only way to know for sure is through proper testing.
Is a rash always a sign of penicillin allergy?
No. A rash that appears days after starting penicillin is often caused by a virus, not the drug. Viral rashes are common during infections like mononucleosis or the flu. If the rash is flat, not itchy, and doesn’t come with swelling or breathing problems, it’s very unlikely to be an allergy.
Can I take amoxicillin if I’m allergic to penicillin?
Amoxicillin is a type of penicillin. If you have a true IgE-mediated penicillin allergy, you should avoid it. But if your allergy label is based on a past rash or stomach upset, you may be able to take amoxicillin safely after testing. Up to 95% of people labeled allergic can tolerate it after proper evaluation.
Is penicillin skin testing painful?
It’s not painful. It’s similar to a allergy test for pollen or peanuts. A tiny drop of penicillin is placed on your skin, then lightly pricked. You might feel a slight sting, but no bleeding. If you’re not allergic, there’s no reaction. If you are, a small bump appears within 20 minutes.
What if I’ve never taken penicillin but my family says I’m allergic?
Family history doesn’t determine penicillin allergy. Allergies aren’t inherited like eye color. If you’ve never had a reaction, you’re not allergic. Don’t assume you are. Get tested if you ever need antibiotics-especially for infections like pneumonia or strep throat, where penicillin is the best option.
Are there alternatives if I’m truly allergic?
Yes. If you have a confirmed penicillin allergy, doctors can use alternatives like cephalosporins (if low-risk), azithromycin, or doxycycline. But these are often less effective, more expensive, and carry higher risks of side effects like C. diff. That’s why testing and de-labeling are so important-even if you’re truly allergic, you might be able to use penicillin safely again.


suhani mathur
Let’s be real-most people think they’re allergic because their kid got a rash after amoxicillin and the doctor just slapped on the label without thinking. I’ve seen it in clinics: parents panic, docs take the easy way out. Ten years later, that kid can’t get a simple infection treated properly because of a misdiagnosis from when they were two. It’s not just ignorance-it’s systemic laziness.
Georgia Brach
The data is cherry-picked. Yes, 80% lose sensitivity over time-but that’s not the same as proving the original diagnosis was wrong. Many of these ‘false positives’ were never formally tested. The CDC’s own guidelines say to assume allergy until proven otherwise. This article reads like pharmaceutical marketing dressed as public health advice.
Payson Mattes
Okay but have you heard about the secret FDA memo from 2017 that says penicillin testing is being pushed because big pharma wants to sell more antibiotics? I know a guy whose cousin works at a lab in Ohio-they’re literally being paid per test. And don’t get me started on how the app PAAT is coded by the same people who make the antibiotics. It’s not about safety-it’s about profit. You think they’d let you test yourself for free if it didn’t boost their bottom line?
Steven Mayer
While the epidemiological correlation between mislabeled penicillin allergies and increased incidence of C. diff and MRSA is statistically significant (p < 0.01), the causal inference remains confounded by comorbidities, prior antibiotic exposure, and hospitalization duration. Moreover, the 2019 mortality study referenced fails to adjust for socioeconomic stratification in antibiotic access. The economic argument-$20 billion annually-is derived from aggregated billing codes, not direct cost-of-care analysis. Until prospective RCTs control for these variables, de-labeling protocols remain heuristic rather than evidence-based.
Diana Alime
ok so i got a rash after penicillin when i was 7 and now im 34 and everyone says im allergic but like… i dont even remember it? and now i need antibiotics for my sinus infection and im scared to ask bc what if i die?? also why does everyone keep saying ‘just get tested’ like its a spa day??
bharath vinay
They want you to believe you’re not allergic because they’re pushing cheaper drugs. But what about the people who *did* have anaphylaxis? What if you test someone who’s been fine for 15 years, and then they drop dead in the clinic? Who takes responsibility? The system is broken, and this is just another way to shift blame onto patients for not jumping through hoops while the real culprits-hospitals, doctors, insurance companies-get richer.
Usha Sundar
My mom was told she was allergic in the 80s. Got tested last year. Turned out she never was. Now she takes penicillin like it’s candy. Saved her from a 3-week hospital stay. Just ask.
claire davies
God, I love how this piece doesn’t just tell you what’s wrong-it gives you a roadmap to fix it. I’m from London, and over here, we’ve got NHS pharmacists doing exactly this-de-labeling folks in 15-minute slots during flu season. One lady came in convinced she’d die if she touched penicillin because her aunt had a ‘bad reaction’ in 1962. Turned out her aunt just got a rash from a virus and was never tested. Now she’s on her third course of amoxicillin in two years and says she feels like she’s been living in a lie. That’s the real win here-not just saving money, but giving people back their trust in their own bodies. We’re so quick to label, but so slow to unlabel. This isn’t just medicine-it’s liberation.