Bladder Training Voiding Tracker
Your Bladder Training Progress
Current Progress
Voiding Log Entries
When the bladder starts firing off involuntary contractions, daily life can feel like a race against a ticking clock. Those sudden urges, painful leaks, and the constant anxiety of not knowing when the next spasm will hit are all hallmarks of urinary tract muscle spasms. The good news? bladder training offers a practical, drug‑free way to retrain the nervous system and calm those noisy muscles.
What Triggers Muscle Spasms in the Urinary Tract?
Muscle spasms in the urinary tract usually originate from the detrusor muscle the smooth muscle that lines the bladder wall and contracts to expel urine. When this muscle becomes over‑active, it sends rapid contraction signals even when the bladder isn’t full. Common culprits include:
- Neurological conditions such as multiple sclerosis or Parkinson’s disease
- Chronic bladder infections that irritate the lining
- Age‑related changes in bladder elasticity
- Certain medications that affect nerve signaling
The resulting condition is often labeled overactive bladder a syndrome marked by urgency, frequency, and sometimes urge incontinence. While pills can help, they don’t address the root cause: the bladder’s habit of contracting too soon.
Defining Bladder Training
Bladder training a structured program that teaches the bladder to hold urine for longer intervals by gradually extending the time between bathroom trips works on the principle of neuro‑plasticity-the brain and nerves can relearn patterns when given consistent cues. By resisting the urge at set intervals, you teach the detrusor muscle that immediate contraction isn’t necessary, which in turn reduces spasms.
How Bladder Training Calms the Detrusor
The process hinges on two physiological tweaks:
- Increasing functional bladder capacity: When you postpone voiding, the bladder stretches gently, signaling to the detrusor that it can hold more urine before it needs to contract.
- Modulating sensory pathways: Repeatedly ignoring a low‑volume urge dulls the afferent nerve signals that trigger premature spasms.
Over weeks, the brain‑bladder loop re‑sets, and the urgency fades.
Step‑by‑Step Guide to Start Bladder Training
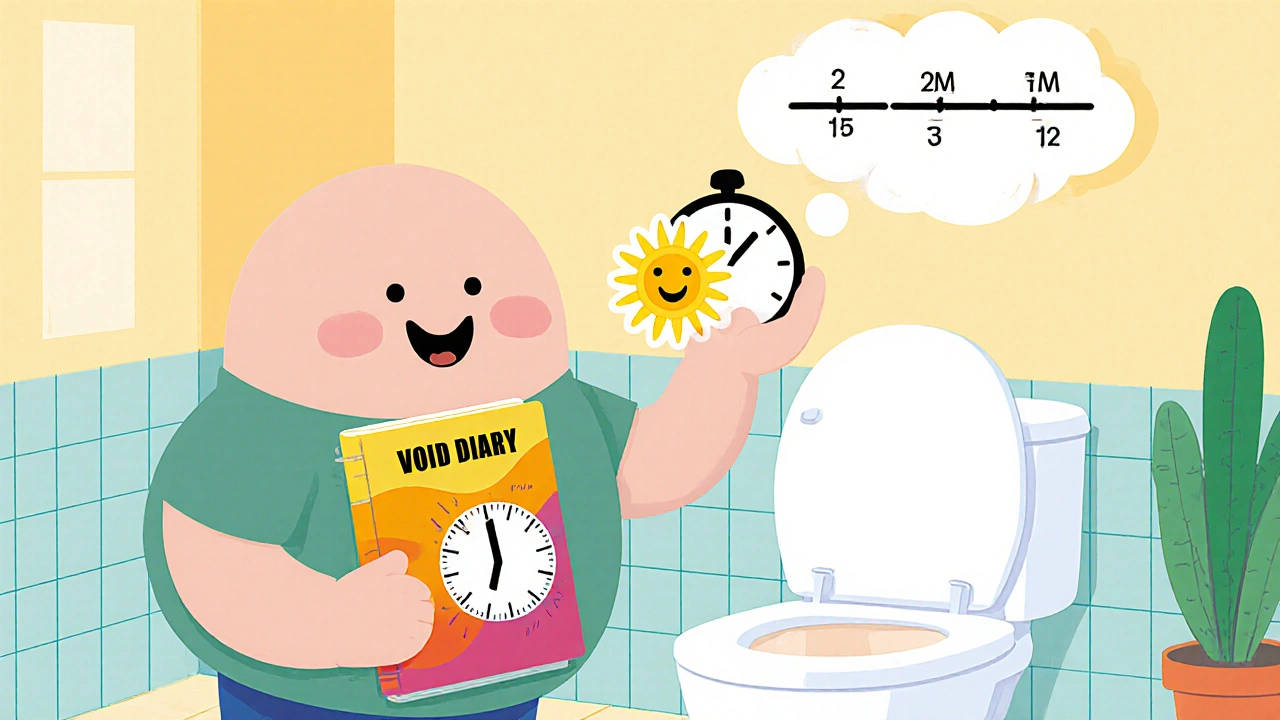
- 1. Keep a voiding diary for three days. Record the time you go, the amount of urine (if you can measure), and any urgency level on a scale of 1‑5.
- 2. Identify your baseline interval. Most adults naturally urinate every 2-3 hours. This becomes your starting point.
- 3. Set a target. Aim to increase the interval by 15‑30 minutes every 3‑4 days, depending on comfort.
- 4. Use a timer. When the clock buzzes, try to hold for the prescribed interval. If urgency spikes, practice a distraction technique (deep breathing, counting, light stretching) for up to two minutes before going.
- 5. Record each attempt in the diary-note successes, failures, and any pain.
- 6. Review weekly. Adjust the interval based on trends: if you consistently succeed, add more time; if you’re constantly failing, stay at the current level until confidence builds.
Patience is key. Most people see a noticeable drop in urgency after four to six weeks of consistent practice.
Complementary Techniques to Boost Success
Bladder training works best when paired with other bladder‑friendly habits.
Pelvic Floor Muscle Strengthening
The pelvic floor muscle a group of muscles that support the bladder, uterus, and bowel acts like a sphincter. Strengthening it improves urge control. The classic Kegel exercise routine is simple:
- Identify the right muscles by stopping urine flow mid‑stream (just for practice, not during the routine).
- Contract for 5 seconds, then relax for 5 seconds. Aim for three sets of 10 reps daily.
Consistent Kegels can reduce leak episodes by up to 30 % in clinical trials.
Biofeedback
Some clinics offer biofeedback a technique that uses sensors to give visual or auditory cues of pelvic floor muscle activity. It helps you fine‑tune contractions, especially if you’re new to Kegels. If you can’t access a clinic, mobile apps with EMG‑compatible pads are a cheap alternative.
Lifestyle Tweaks
- Limit caffeine and alcohol, both of which irritate the bladder lining.
- Stay hydrated but avoid gulping large volumes at once; sip water throughout the day.
- Maintain a healthy weight-excess pressure on the pelvis can worsen spasms.
- Practice timed voiding after meals (the “gastro‑colic reflex” can trigger a bladder contraction).
When‑to‑Consider Medication or Other Therapies
Bladder training isn’t a magic bullet for everyone. Severe overactive bladder may require pharmacologic support. Below is a quick comparison of common approaches.
| Aspect | Bladder Training | Anticholinergic Medication | Intermittent Catheterization |
|---|---|---|---|
| Primary Goal | Increase bladder capacity & reduce urgency | Relax detrusor muscle chemically | Directly empty bladder to avoid over‑distension |
| Typical Onset of Relief | 4‑6 weeks of consistent practice | 1‑2 weeks after starting dose | Immediate after each catheterization |
| Side‑Effect Profile | None (except occasional frustration) | Dry mouth, constipation, blurred vision | Urinary tract infection risk |
| Long‑Term Sustainability | High if habit maintained | May require dose tapering | Requires regular equipment and technique |
If you’re unsure which route to take, discuss your diary results with a urologist or continence nurse. They can tailor a plan that blends training with low‑dose medication for faster relief.

Common Pitfalls and How to Overcome Them
- Giving up after a few setbacks: Urgency spikes are normal. Record the incident, note the trigger, and resume the schedule the next day.
- Skipping the diary: Without data you can’t see progress. Even a simple phone note counts.
- Holding too long, too quickly: Increase intervals gradually; aggressive jumps can cause painful bladder over‑stretch.
- Ignoring pelvic floor health: Weak muscles make it harder to suppress urges. Pair training with Kegels for best results.
- Relying solely on caffeine‑free diet: Lifestyle changes help but won’t replace the training habit.
Addressing these issues early keeps motivation high and speeds up the calming of those pesky spasms.
Quick Checklist for Successful Bladder Training
- Log every void for at least three days.
- Identify your natural interval (usually 2‑3 hrs).
- Set realistic extension goals (15‑30 min increments).
- Use a timer and distraction techniques.
- Practice Kegel exercises daily.
- Review diary weekly and adjust the plan.
- Seek professional advice if urgency persists after 8 weeks.
Frequently Asked Questions
How long does it take to see results from bladder training?
Most people notice a reduction in urgency after four to six weeks of consistent practice, though full bladder‑capacity gains may take up to three months.
Can I do bladder training if I have a urinary tract infection (UTI)?
It’s best to treat the infection first. An active UTI can heighten sensitivity, making training less effective and more uncomfortable.
Do I need special equipment for bladder training?
No. All you need is a timer or smartphone alarm, a notebook (or an app) for tracking, and optionally a biofeedback device if you want extra guidance.
What if I keep having sudden leaks despite training?
Persistent leakage may signal an underlying condition such as bladder stones, prostate enlargement, or nerve damage. Consult a urologist for further evaluation.
Is bladder training safe for older adults?
Yes. Age‑related changes often make the bladder more reactive, so a gentle, progressive training program is especially beneficial for seniors.

nitish sharma
The comprehensive bladder‑training protocol you presented showcases a methodical progression from baseline assessment to interval expansion, which aligns with established neuro‑plasticity principles. By emphasizing a voiding diary, patients gain quantitative feedback that can reinforce adherence. The inclusion of pelvic‑floor strengthening as an adjunct is particularly prudent, given its documented impact on detrusor inhibition. Overall, the structured timeline offers a realistic framework for both clinicians and sufferers.
Rohit Sridhar
Embarking on bladder training can indeed feel daunting at first, but the gradual nature of the program ensures that the nervous system is not shocked into dysfunction. Starting with a three‑day voiding diary provides a clear baseline, allowing you to identify your natural interval without speculation. Once that baseline is established, extending the interval by fifteen to thirty minutes every few days creates a gentle stretch on the detrusor muscle, encouraging it to accommodate larger volumes. The timer serves as an external cue, reinforcing the internal schedule you are teaching your bladder. When an urge spikes, employing distraction techniques-such as deep breathing, counting backwards, or light stretching-helps to modulate the afferent signals that trigger premature contractions. Consistent practice over four to six weeks typically yields a noticeable reduction in urgency, as the brain‑bladder loop recalibrates its response thresholds. It is essential to record every attempt, noting successes, setbacks, and any associated discomfort, because this data drives iterative adjustments. If you find yourself repeatedly failing at a particular interval, maintain that level until confidence builds before progressing further. The synergy between bladder training and pelvic‑floor exercises cannot be overstated; Kegel contractions performed in tandem provide additional support for urge suppression. Moreover, lifestyle tweaks such as limiting caffeine and alcohol, staying hydrated with steady sips, and maintaining a healthy weight contribute to overall bladder health. Biofeedback devices, while optional, can offer visual reinforcement of correct muscle engagement, especially for beginners. In cases where overactive bladder symptoms persist despite diligent training, a low‑dose anticholinergic may be introduced under medical supervision to accelerate relief. However, medication should complement-not replace-the behavioral foundation you have established. Remember that setbacks are normal; the key is to resume the schedule promptly after each incident. Ultimately, the goal is to empower you to regain control over your urinary patterns, reducing anxiety and improving quality of life. Consistency, patience, and attentive self‑monitoring form the triad of success in bladder training.
Nhasala Joshi
🚨⚠️ The covert agenda behind “bladder training” is nothing short of a systemic mind‑control operation, exploiting neuro‑plasticity to condition citizens into silent compliance with elite urinary protocols. ⏰ The timer is a metronomic beacon, synchronizing peripheral detrusor activity with hidden biometric networks that harvest involuntary data streams. 🧬 By perpetually modulating afferent pathways, the regime subtly rewires the somatic‑autonomic axis, enabling the shadow pharmaco‑industrial complex to monetize compliance via optional biofeedback accessories. 😱 Every Kegel contraction becomes a data point in a clandestine ledger, feeding algorithmic predictions that could be weaponized for behavioral manipulation. 📉 The tables they present are sanitized, but the underlying calculus is a relentless drive toward population‑level bladder homogenization, eroding individual physiological autonomy. 💥
Joe Moore
i cant believe these tips actually work lol.
Ayla Stewart
It is encouraging to hear that the suggested methods have produced tangible improvements for some individuals.
Poornima Ganesan
Your reliance on diary entries, while a commendable start, overlooks the significance of precise uroflowmetry measurements that can more accurately gauge detrusor dynamics. Integrating uro‑dynamic studies early in the protocol would allow for stratified interventions, distinguishing neurogenic overactivity from myogenic dysfunction. Moreover, the recommendation to increase intervals by fifteen minutes indiscriminately fails to account for bladder compliance variability across patients. A tailored approach, calibrated to individual capacity curves, mitigates the risk of over‑distension and subsequent pain. Ignoring these nuances reduces the program to a one‑size‑fits‑all regimen, which may inadvertently exacerbate symptoms in a subset of users.
Janet Morales
While your emphasis on high‑tech diagnostics sounds impressive, the everyday patient does not have access to a uroflowmeter hidden in a laboratory, and insisting on such equipment only fuels elitist gatekeeping. The reality is that consistent behavioral training, even without sophisticated measurements, yields meaningful relief for the vast majority of sufferers. Overcomplicating the regimen with unnecessary jargon alienates the very community that needs simple, actionable guidance. Therefore, the pragmatic, low‑cost approach you dismiss should be celebrated, not condemned.
Tracy O'Keeffe
Honestly, the prosaic enumeration of intervals and Kegel sets you’ve supplied reads like a pedestrian treadmill plan, bereft of the avant‑garde bio‑feedback symphonies that truly reprogram the detrusor’s chaotic opera. One must transcend the banal “fifteen‑minute” increments and embrace harmonic resonance training-think pulsatile auditory cues synchronized with cortical entrainment modules. Such high‑octane methodologies, albeit unorthodox, shatter the conventional shackles of bladder management, propelling the practitioner into a realm where urinary control becomes a trans‑dimensional artform. If you’re content with mediocrity, stick to the spreadsheet; if you crave quantum‑level mastery, seek the clandestine clinics that fuse neuro‑stimulation with poetic respiration.