When you’re trying to manage type 2 diabetes and lose weight at the same time, most medications make one goal harder. Insulin? It often makes you gain weight. Metformin? Helps a little with weight but doesn’t move the needle much. Sulfonylureas? Almost guaranteed to pack on pounds. But GLP-1 receptor agonists are different. They don’t just control blood sugar-they help you lose significant weight, sometimes more than 15% of your body weight, while lowering your A1c by nearly 2%. That’s not a side effect. It’s the point.
How GLP-1 Agonists Actually Work
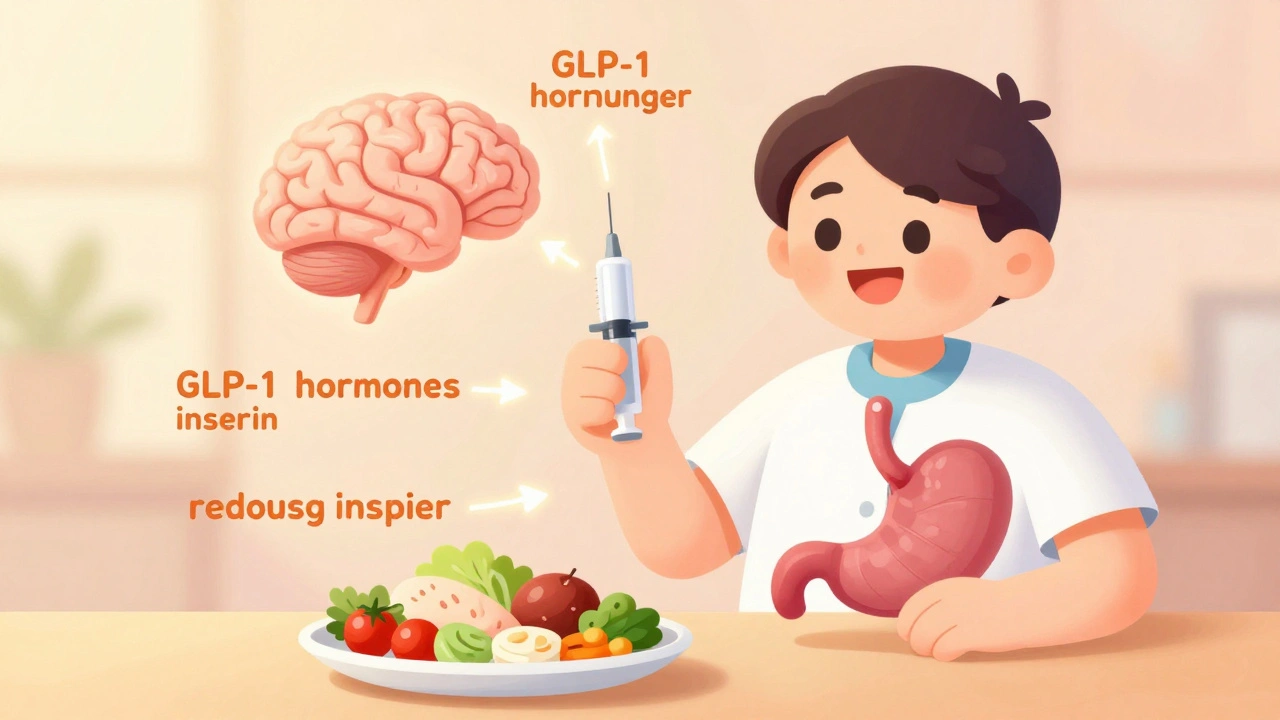
These drugs mimic a hormone your body already makes-glucagon-like peptide-1, or GLP-1. It’s released after you eat, signaling your pancreas to release insulin, telling your brain you’re full, and slowing down how fast food leaves your stomach. GLP-1 receptor agonists amplify all of that.
When you inject semaglutide, liraglutide, or tirzepatide, you’re not just tricking your body. You’re supercharging a natural system. The drug binds to receptors in your pancreas, boosting insulin only when your blood sugar is high-so you rarely get low blood sugar. It also shuts down glucagon, the hormone that tells your liver to dump more sugar into your bloodstream. That alone can drop your fasting glucose by 20-30%.
But the real game-changer is what happens in your brain. GLP-1 receptors in the hypothalamus turn down hunger signals. Studies show they reduce cravings for high-fat, high-sugar foods by 30-40%. People on these drugs often say, “I don’t feel hungry anymore.” Not because they’re starving themselves. Because their brain stopped screaming for junk food. One Reddit user wrote, “I used to snack at 2 a.m. Now I just don’t think about it.”
And then there’s the gut. Slowing gastric emptying by 15-30% means sugar enters your bloodstream slowly. No spikes. No crashes. That’s why A1c-a measure of average blood sugar over 3 months-drops so consistently. In clinical trials, semaglutide at 1.0 mg weekly lowered A1c from 8.7% to 6.9%. That’s not just better control. That’s moving from prediabetes range to normal.
Weight Loss Numbers That Actually Matter
Let’s talk numbers. Not vague promises. Real data from real trials.
Take semaglutide (Wegovy) at 2.4 mg weekly. In the STEP 8 trial, people lost an average of 15.8% of their body weight over 68 weeks. That’s not “a few pounds.” That’s 30-40 pounds for most people. And 50% lost 15% or more. Compare that to liraglutide (Saxenda) at 3.0 mg daily: 6.4% weight loss. Or placebo: 2.4%.
Tirzepatide (Zepbound), a newer dual GLP-1 and GIP agonist, is even stronger. In the SURMOUNT-1 trial, people on the highest dose (15 mg) lost 20.2% of their body weight. That’s close to what you’d see after gastric bypass surgery. And it’s not just fat. Muscle mass stayed mostly intact.
But here’s the catch: you have to stay on it. When people stop, they regain 50-70% of the weight within a year. That’s not failure. It’s biology. Your body fights to return to its old weight. GLP-1 agonists don’t fix your metabolism. They temporarily reset your appetite control system. If you stop, your brain reverts.
How They Compare to Other Diabetes Drugs
Here’s a quick comparison:
| Medication | A1c Reduction | Average Weight Change | Dosing |
|---|---|---|---|
| Semaglutide (Ozempic/Wegovy) | 1.8% | -14.9% to -15.8% | Once weekly |
| Tirzepatide (Mounjaro/Zepbound) | 2.0-2.4% | -20.2% | Once weekly |
| Liraglutide (Victoza/Saxenda) | 1.1-1.2% | -6.4% | Once daily |
| Dulaglutide (Trulicity) | 1.0-1.5% | -5.5% | Once weekly |
| Metformin | 0.5-1.0% | -2 to -3 kg | Twice daily |
| Insulin | 1.0-1.5% | +4 to +10 kg | Once or more daily |
| Sitagliptin (DPP-4 inhibitor) | 0.5-1.0% | ±0.5 kg | Once daily |
GLP-1 agonists are the only class that consistently beats insulin and sulfonylureas on both metrics. And unlike SGLT2 inhibitors (like empagliflozin), which cause weight loss by making you pee out sugar, GLP-1 drugs work by changing how you feel about food. That’s why they’re now first-line for people with type 2 diabetes who also have obesity.

Side Effects: The Trade-Off
They’re not magic pills. About half of people experience nausea, especially in the first 4-8 weeks. Vomiting happens in 5-10%. Diarrhea and constipation are common too. But most of these fade as your body adjusts.
The key is slow titration. Semaglutide starts at 0.25 mg once a week for a month. Then it goes to 0.5 mg, then 1.0 mg, then 1.7 mg, and finally 2.4 mg. Rushing this increases side effects. Most people who quit early do so because they jumped the dose too fast.
Doctors recommend starting at the lowest dose and waiting at least 4 weeks between increases. Take it at night if nausea hits hard. Avoid greasy or heavy meals during the first few weeks. Over-the-counter meds like dimenhydrinate (Dramamine) can help if nausea is bad.
Needle anxiety? Normal. Most people get used to it after 2-3 injections. The pens are small, fine needles, and many now have hidden needles or auto-injectors. A 2022 survey found 85% of patients were comfortable self-injecting after training.
Cost and Access: The Real Barrier
Without insurance, these drugs cost $800-$1,200 a month in the U.S. That’s why so many people can’t access them. Medicare Part D covers about 62% of prescriptions-but only after you’ve tried and failed other weight-loss meds. Private insurers often require a BMI over 30, documentation of failed diet attempts, or proof of diabetes.
Some patients use pharmacy discount cards. Others travel to Canada or Mexico for lower prices. A few get access through clinical trials. But the truth? The system is still catching up to how effective these drugs are.
Novo Nordisk, maker of Ozempic and Wegovy, made $10.8 billion in 2023 from these drugs alone. Demand is so high that the FDA still lists semaglutide as in shortage. That’s not a glitch. It’s a sign that millions are benefiting.

What Happens After You Stop?
This is the question no one asks until it’s too late. If you stop taking the drug, your appetite returns. Your stomach empties faster. Your brain forgets what full feels like. And you regain weight-fast.
Studies show most people regain over half their lost weight within a year of stopping. That’s why experts say these aren’t “weight loss drugs.” They’re “weight management drugs.” Like blood pressure medication, you often need to take them long-term.
Some people try to wean off slowly. Others switch to lifestyle changes-high protein, low sugar, strength training. But the data is clear: without ongoing pharmacological support, the body reverts.
The Future: Beyond Weight and A1c
These drugs are doing things no one expected. In the STEP-HFpEF trial, semaglutide improved heart failure symptoms in obese patients-even without diabetes. In the ENCHANT trial, it cut liver fat by over 50% in people with fatty liver disease. Novo Nordisk is now testing it for Alzheimer’s prevention, because GLP-1 receptors are found in the brain, and inflammation plays a role in dementia.
Tirzepatide is just the start. Triple agonists (GLP-1 + GIP + glucagon) are in phase 2 trials. Oral versions are coming. One oral semaglutide pill is already approved for diabetes, and a higher-dose version for weight loss is expected by 2026.
But here’s the bottom line: GLP-1 receptor agonists aren’t just another pill. They’re a new way of treating metabolic disease. They don’t just lower numbers. They change how you experience hunger, food, and your own body.
Do GLP-1 agonists cure diabetes?
No. They manage type 2 diabetes by improving insulin sensitivity, reducing liver sugar output, and slowing digestion. Many people see their A1c drop into the normal range, but if they stop the drug, blood sugar usually rises again. They’re not a cure-they’re a long-term management tool.
Can I take GLP-1 agonists if I don’t have diabetes?
Yes. Wegovy and Zepbound are FDA-approved for chronic weight management in adults with a BMI of 30 or higher, or 27 or higher with at least one weight-related condition like high blood pressure or sleep apnea. You don’t need diabetes to qualify.
How long does it take to see results?
Most people notice reduced appetite within the first week. Weight loss typically starts after 4-6 weeks. The biggest drops happen between months 3 and 6. A1c usually drops by 1% within 12 weeks. Full effects take 16-20 weeks, especially with slow titration.
Are there any long-term risks?
So far, the long-term safety profile looks good. The LEADER trial showed liraglutide reduced heart attacks and strokes by 13% in high-risk patients. However, rare side effects include gallbladder disease and pancreatitis. The FDA is monitoring potential links to thyroid tumors in rodents, but no such risk has been confirmed in humans. Regular check-ups are recommended.
Can I drink alcohol while on GLP-1 agonists?
Moderate alcohol is generally okay, but it can increase nausea and lower blood sugar, especially if you’re also on insulin or sulfonylureas. Alcohol also adds empty calories, which can slow weight loss. Most doctors recommend limiting alcohol during the first few months while your body adjusts.
What’s Next?
If you’re considering one of these drugs, talk to your doctor about your goals. Are you trying to get off insulin? Lower your A1c below 7%? Lose 10% of your body weight? Be specific. These drugs work best when you know why you’re taking them.
Don’t expect overnight results. Don’t expect no side effects. But do expect a tool that can change your relationship with food-and your health-in ways few other medications can.

Linda Migdal
Let’s be real - these drugs are just fancy appetite suppressants wrapped in medical jargon. The FDA approved them because Big Pharma pushed them hard, not because they’re revolutionary. We’re trading one dependency for another. And don’t even get me started on the $1,200/month price tag while millions go without insulin. This isn’t healthcare - it’s a luxury market dressed up as science.
Tommy Walton
It’s not about weight. It’s about being. 🌱 GLP-1 agonists don’t just alter biology - they dissolve the illusion of willpower. We’re not broken. We’re overstimulated. These drugs? They’re the quiet rebellion against a food system designed to make you crave chaos. 🧠✨
Kshitij Shah
Bro, in India we’ve been eating curry and rice for 5000 years and never needed a $1000 shot to feel full. Now everyone’s obsessed with ‘resetting their brain.’ Meanwhile, my aunt lost 20kg by just walking after dinner and not eating sweets after 8pm. 🤷♂️ Maybe we’re overcomplicating this?
Sean McCarthy
Weight loss data is misleading. People say 15% loss but they don’t mention the muscle loss. Also nausea is not just 'common' - it's debilitating for many. And the rebound weight gain? That's not biology. That's the system failing you after selling you a dream.
Bee Floyd
I’ve been on semaglutide for 11 months. The first month was rough - nausea, headaches, feeling like my stomach was full of lead. But by month three, I stopped craving donuts. Not because I was strong. Because my brain stopped screaming. I didn’t 'decide' to eat less. I just… didn’t want to. It’s weird. And kind of beautiful. Still, I’m not calling it a cure. Just a pause button on my old habits.
Jeremy Butler
It is incumbent upon the medical community to recognize that pharmacological intervention in the realm of metabolic regulation constitutes a paradigmatic shift in therapeutic ontology. The ontological reconfiguration of homeostatic appetite regulation via GLP-1 receptor agonism represents not merely a pharmacological advance, but a metaphysical recalibration of human agency vis-à-vis biological determinism.
Souvik Datta
Look, I get it - these drugs are powerful. But don’t let the hype make you forget the basics: movement, sleep, stress management. I’ve helped 12 patients on GLP-1s. Five of them started walking daily, cooking at home, and sleeping better. Guess what? Their results got even better. The drug isn’t the hero. It’s the catalyst. You still have to show up.
Irving Steinberg
So basically you're saying we should pay a grand a month to not feel hungry? Meanwhile my cousin lost 80 lbs on keto and never touched a needle. I'm just saying… maybe we're all just lazy and want a magic button 🤷♂️😂
Adrian Barnes
The data is cherry-picked. The trials exclude patients with comorbidities. The long-term cardiovascular outcomes are not yet established. The pharmaceutical marketing machine has weaponized patient desperation. This is not medicine. It is commodified hope wrapped in clinical trial language. Proceed with extreme caution - and skepticism.
soorya Raju
you think this is about weight? nah its a secret gov plan to control us via the brain. the FDA is owned by novonordisk and the needles have microchips. i saw a guy on youtube who said his dog started talking after he took it. also the 20% weight loss? fake. its all CGI. theyre replacing our souls with algorithms. also i think the moon is made of cheese