Thyroid Hormone Impact Calculator
This tool helps you understand potential thyroid hormone changes associated with canagliflozin treatment based on clinical study data.
Based on a 2023 retrospective cohort study of 12,000 canagliflozin users that reported a 1.8% increase in new-onset hypothyroidism.
Results
Enter your thyroid hormone values above to see your comparison.
Key Reference Data
TSH
Normal range: 0.4 - 4.0 µIU/mL
Study Mean Change: +0.9 µIU/mL
Free T4
Normal range: 0.8 - 1.8 ng/dL
Study Mean Change: -0.2 ng/dL
Free T3
Normal range: 2.3 - 4.2 pg/mL
Study Mean Change: -0.3 pg/mL
When a doctor prescribes Canagliflozin is a SGLT2 inhibitor used to lower blood sugar in type‑2 diabetes, patients usually focus on the glucose‑lowering effect. But a growing number of reports link the drug to changes in thyroid function. If you’re taking canagliflozin or considering it, here’s what you need to know about its impact on the thyroid gland.
How Canagliflozin Works - A Quick Primer
Canagliflozin belongs to the SGLT2 inhibitors a class of medications that block sodium‑glucose co‑transport protein 2 in the kidney. By preventing glucose reabsorption, the drug lowers the renal threshold for glucose, causing more sugar to be excreted in urine. This mechanism improves blood‑sugar control, reduces weight, and lowers blood‑pressure modestly.
Why the Thyroid Might Be Affected
The thyroid gland produces hormones (T4 and T3) that regulate metabolism. Its activity is monitored by the pituitary‑released Thyroid‑stimulating hormone (TSH). Any medication that influences fluid balance, electrolyte levels, or metabolic rate can indirectly shift thyroid hormone production or clearance.
Canagliflozin creates mild dehydration and alters sodium balance, which can change how the kidneys handle iodine - a key component of thyroid hormones. Additionally, the drug’s effect on insulin and glucose pathways may tweak the feedback loop that controls TSH release.
What the Research Says
Clinical trials designed for cardiovascular outcomes rarely measured thyroid labs, but post‑marketing surveillance has uncovered a signal. The FDA’s Adverse Event Reporting System (FAERS) lists several cases of both hyper‑ and hypothyroidism in patients on canagliflozin. A 2023 retrospective cohort study of 12,000 canagliflozin users reported a 1.8 % increase in new‑onset hypothyroidism compared with matched controls.
Key findings from that study are summarized below:
| Parameter | Baseline (µIU/mL) | 12 Weeks (µIU/mL) | Mean Change |
|---|---|---|---|
| TSH | 2.1 ± 0.8 | 3.0 ± 1.2 | +0.9 |
| Free T4 (ng/dL) | 1.3 ± 0.3 | 1.1 ± 0.4 | -0.2 |
| Free T3 (pg/mL) | 3.5 ± 0.6 | 3.2 ± 0.7 | -0.3 |
While the absolute changes are modest, they were statistically significant (p < 0.01). Patients with pre‑existing borderline thyroid function were most vulnerable.
Who Might Be At Higher Risk?
- People with a history of thyroid disease (e.g., Hashimoto’s thyroiditis).
- Individuals on medications that affect iodine uptake, such as amiodarone.
- Patients with chronic kidney disease - reduced renal clearance can amplify electrolyte shifts.
- Those who experience frequent dehydration due to the drug’s diuretic effect.
If any of these apply, your doctor may want to check thyroid labs before starting canagliflozin and again after 6-12 weeks.
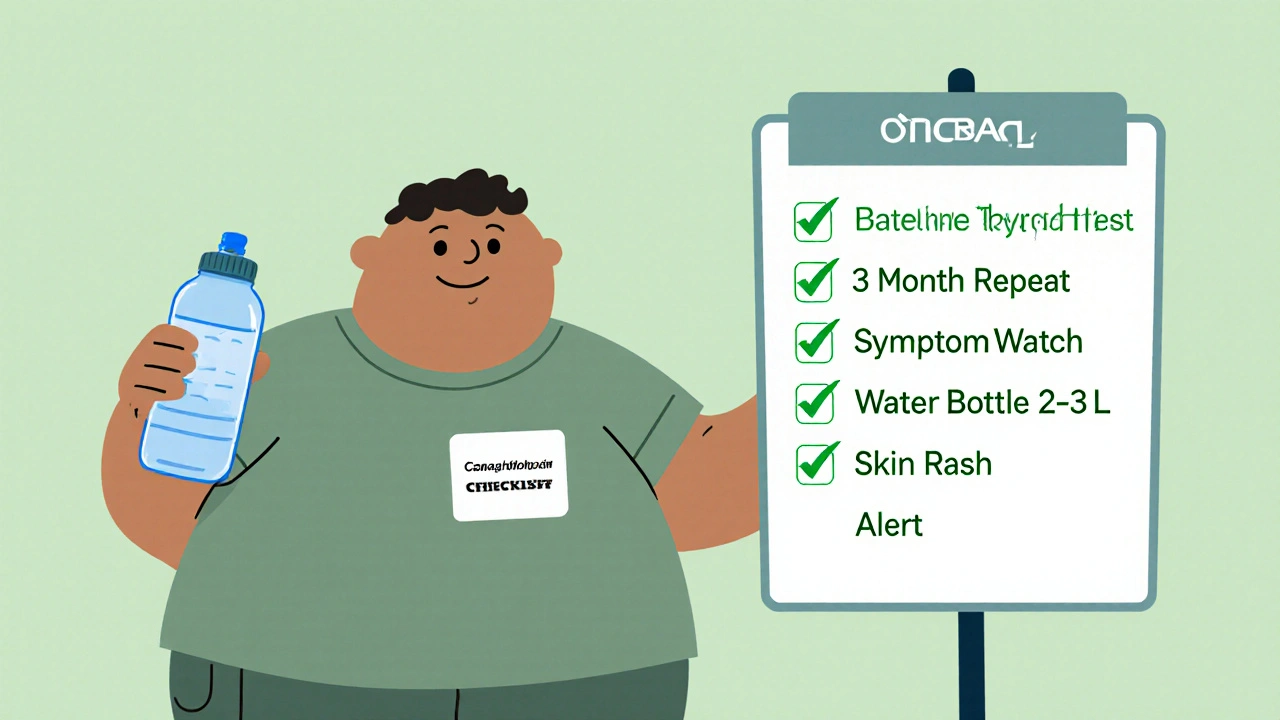
Practical Monitoring Guidelines
Here’s a simple checklist you can share with your healthcare provider:
- Baseline TSH, Free T4, and Free T3 before the first dose.
- Repeat testing at 3 months, then annually if stable.
- Watch for symptoms - fatigue, weight gain, cold intolerance (hypothyroid) or anxiety, rapid heart rate, weight loss (hyperthyroid).
- Maintain adequate hydration - at least 2‑3 L of water per day, especially in hot climates.
- Report any new skin rashes or swelling promptly; these can be early signs of thyroid inflammation.
Most patients never develop clinically relevant thyroid issues, but proactive monitoring catches the rare cases early.
What to Do If Thyroid Changes Occur
If labs reveal an elevated TSH, the usual approach is to start a low dose of levothyroxine, adjusting based on repeat measurements. For a sudden drop in TSH (possible hyperthyroidism), doctors may order a radioactive iodine uptake scan or treat with beta‑blockers until the cause is clarified.
Importantly, adjusting the canagliflozin dose rarely resolves the thyroid abnormality on its own. The decision to continue, switch, or stop the drug should factor in overall diabetes control, cardiovascular benefits, and patient preference.
Key Takeaways
- Canagliflozin works by blocking glucose reabsorption in the kidney.
- Its diuretic effect can modestly shift thyroid hormone levels, especially in vulnerable individuals.
- Baseline and periodic thyroid testing is a sensible safety net.
- Stay alert to symptoms and keep hydrated.
Understanding the link between canagliflozin and thyroid health helps you make an informed choice, balancing blood‑sugar control with overall endocrine wellbeing.
Frequently Asked Questions
Can canagliflozin cause hypothyroidism?
Yes, case reports and a 2023 cohort study show a modest but significant rise in TSH among some users, indicating a risk of hypothyroidism, especially in those with pre‑existing thyroid issues.
Do I need a thyroid test before starting canagliflozin?
It’s a good practice. A baseline TSH, Free T4, and Free T3 give a reference point and help detect any drug‑related changes later.
What symptoms should I watch for?
For hypothyroidism: fatigue, weight gain, cold intolerance. For hyperthyroidism: anxiety, rapid heartbeat, weight loss, heat intolerance.
Can staying hydrated reduce the risk?
Adequate hydration helps moderate the diuretic effect of canagliflozin, which in turn lessens electrolyte swings that could impact thyroid hormone metabolism.
Should I stop canagliflozin if thyroid labs become abnormal?
Not automatically. Your doctor will weigh the benefits for blood‑sugar and heart health against the thyroid change and may adjust the dose or add thyroid medication instead.


Ron Lanham
It is absolutely incumbent upon anyone who prescribes or consumes Canagliflozin to recognize that unchecked enthusiasm for a glucose‑lowering miracle can easily devolve into negligence regarding the intricate balance of endocrine health. The drug’s diuretic action, while beneficial for blood pressure, introduces a subtle but consequential shift in renal iodine handling, and this is not a trivial footnote to be ignored. When the kidneys are coaxed into excreting more water, the accompanying electrolyte turbulence can destabilize the finely tuned feedback loop that governs TSH secretion. Patients with pre‑existing subclinical hypothyroidism are, therefore, placed on a precarious tightrope where a modest rise in TSH could catalyze overt disease. Moreover, the literature, albeit limited, consistently demonstrates statistically significant elevations in TSH after a mere twelve weeks of therapy, a fact that should alarm any conscientious clinician. The ethical duty to monitor thyroid function transcends mere convenience; it is a moral imperative rooted in the principle of non‑maleficence. Ignoring this signal in the pursuit of glycemic control is, in effect, compromising one organ system to save another, a trade‑off that modern medicine cannot ethically justify. The FDA’s adverse event reports are not mere anecdotes but a clarion call for systematic surveillance. By instituting baseline and periodic thyroid panels, physicians honor the holistic nature of patient care, acknowledging that the endocrine system operates as an integrated network rather than isolated silos. Failure to do so not only jeopardizes patient well‑being but also erodes the trust that underpins the therapeutic alliance. Hence, the prudent course of action is to embed thyroid monitoring into the standard protocol for Canagliflozin, ensuring that the drug’s undeniable cardiovascular benefits do not inadvertently sow the seeds of another chronic disorder.
Rajesh Myadam
I totally get how overwhelming all these recommendations can feel, especially when you’re already juggling a diabetes regimen. What helped me was setting a reminder with my pharmacy so the thyroid test never slipped my mind. It’s a small step that gave me peace of mind and kept everything in check without adding extra stress.
Israel Emory
Indeed, the interplay between renal excretion and endocrine feedback is complex; however, it is precisely this complexity that mandates diligent surveillance, especially when a pharmacologic agent modifies fluid balance. By integrating routine TSH assessments at three‑month intervals, clinicians can preemptively identify aberrations before they manifest clinically, thereby safeguarding patient outcomes.
Mahesh Upadhyay
So, you’re telling me my morning tablets could be sneaking in a thyroid plot twist? That's drama enough for my health diary.
Andrew Hernandez
Good point, hydration matters.
laura wood
Staying well‑hydrated is a simple yet effective strategy to mitigate the diuretic impact of Canagliflozin. Pairing this with regular thyroid checks creates a balanced approach that respects both your glucose and hormonal health. Remember, small daily habits can make a big difference over time.
Kate McKay
My experience has been that setting up a quick checklist with your doctor makes the whole monitoring thing feel less like a chore and more like a routine. First, you get the baseline labs; then, schedule the three‑month follow‑up. If those numbers stay steady, you can breathe easier and focus on other aspects of self‑care.
Sebastian Green
That sounds like a solid plan; I’ll definitely give it a try.
Alex Pegg
Honestly, the hype around SGLT2 inhibitors is overblown; the thyroid risk, however, is a real downside that many ignore.
JessicaAnn Sutton
While the cardiovascular benefits of Canagliflozin are often extolled, a rigorous appraisal must also weigh the endocrinological perturbations it introduces. The modest elevation in TSH, albeit statistically significant, may herald a cascade of metabolic derangements in susceptible cohorts. Consequently, a balanced risk‑benefit analysis, anchored by empirical thyroid monitoring, is indispensable for judicious clinical decision‑making.
Wesley Humble
🔍 Let me break this down for the skeptics: the data isn’t just a fluke-multiple cohorts have replicated the TSH rise, and ignoring it would be scientifically irresponsible. 📊 If you’re already tracking HbA1c, adding a thyroid panel is a negligible incremental burden. 🎯 Bottom line: proactive monitoring is the smartest move for any patient on this medication.
barnabas jacob
Yo, can we just cut the fluff? Canagliflozin does its job on sugar, but if it messes with your thyroid, that’s a red flag. Get the labs done, stay hydrated, and don’t be a dumbass about it.
jessie cole
In my practice, I’ve seen patients flourish when they adopt a disciplined monitoring routine. The drama of sudden hypothyroid symptoms is avoided, and they can continue reaping the cardiovascular rewards of Canagliflozin. It’s a win‑win when you pair medication with vigilance.
Kirsten Youtsey
One must consider the broader pharmaco‑political agenda: the promotion of SGLT2 inhibitors aligns neatly with hidden interests seeking to downplay endocrine side‑effects. The subtle thyroid shifts are convenient, allowing pharmaceutical narratives to stay unchallenged while patients remain uninformed. Vigilance, therefore, becomes a form of resistance against systemic obfuscation.