When your skin breaks out in thick, red, scaly patches, it’s easy to think it’s just a cosmetic issue. But if you also notice your fingers or toes swelling like sausages, your heels hurting when you walk, or your lower back stiffening up in the morning, you’re not just dealing with a skin problem. You might be facing psoriatic arthritis - a hidden, systemic autoimmune disease that attacks both your skin and your joints.
What Exactly Is Psoriatic Arthritis?
Psoriatic arthritis (PsA) doesn’t show up out of nowhere. It almost always follows psoriasis - a chronic skin condition where the immune system speeds up skin cell growth, causing plaques to build up. About 30% of people with psoriasis will develop PsA, according to the American College of Rheumatology’s 2022 guidelines. In 85% of those cases, the skin symptoms come first. But in 5 to 10% of people, joint pain starts before any visible rash appears. That’s why doctors now check for joint issues even in people with mild psoriasis. The real problem isn’t just the plaques or the swollen joints. It’s what’s happening inside. Your immune system, which is supposed to protect you from viruses and bacteria, turns against your own body. It mistakes healthy skin cells and joint tissues for invaders. This triggers inflammation that doesn’t shut off. Over time, that constant inflammation eats away at cartilage, erodes bone, and damages tendons where they attach to bone - a condition called enthesitis.How PsA Shows Up: More Than Just Rashes and Aching Joints
PsA doesn’t present the same way in everyone. It’s not one disease - it’s a group of symptoms that can hit different parts of your body at different times.- Joint pain and swelling: Often affects the small joints of fingers and toes, but can also hit knees, ankles, and the spine. The swelling isn’t always symmetrical like in rheumatoid arthritis - it might only be in one hand, or just one knee.
- Dactylitis: Also called "sausage digits," this is when an entire finger or toe swells up uniformly. It’s a hallmark sign of PsA and happens in about 40% of patients.
- Enthesitis: Pain where tendons or ligaments meet bone. The Achilles tendon and the bottom of the foot are common spots. Walking can feel like stepping on gravel.
- Nail changes: Pitting, ridges, thickening, or nails lifting off the nail bed. Up to 80% of people with PsA have these changes - more than in any other joint disease.
- Spinal involvement: About 40% of people develop inflammation in the spine (spondylitis), leading to stiffness in the lower back or neck, especially in the morning.
And yes - the skin plaques are still there. Red, raised patches with silvery scales, usually on elbows, knees, scalp, and lower back. But here’s the catch: the severity of your skin rash doesn’t match the severity of your joint damage. Someone with mild psoriasis can have severe joint erosion, and someone with thick plaques might have only minor joint pain.
How Do Doctors Diagnose It?
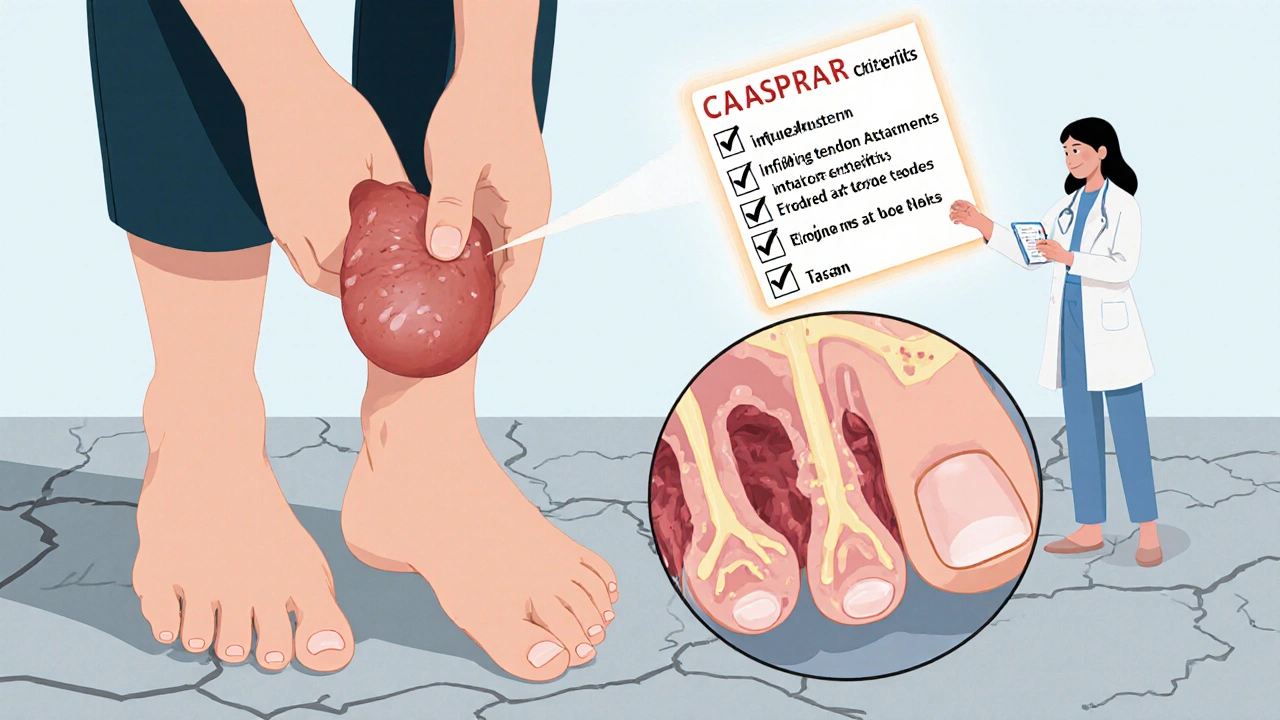
There’s no single blood test for PsA. Diagnosis relies on connecting the dots between symptoms, physical exams, imaging, and lab results. The gold standard is the CASPAR criteria, developed in 2006 and still used today. To meet the criteria, you need inflammatory joint disease plus at least three of these:- Current psoriasis (3 points)
- History of psoriasis (2 points)
- Psoriatic nail changes (1 point)
- Negative rheumatoid factor (1 point)
- Characteristic bone changes on X-ray (1 point)
A score of 3 or more confirms PsA. That’s why doctors don’t just look at your joints - they check your nails, ask about family history (since psoriasis often runs in families), and order imaging.
X-rays show bone erosion in 60-70% of people with long-standing PsA. But newer tools like ultrasound and MRI can spot inflammation before any damage appears. That’s critical - catching PsA early means you can stop the damage before it’s permanent.
What’s Driving the Disease?
Genetics play a big role. If you have a close relative with psoriasis or PsA, your risk goes up. Specific genes like HLA-B27, HLA-B38, and HLA-B39 are strongly linked to PsA. But genes alone don’t cause it. Something has to trigger it - and that’s where environment comes in.Stress, infections (like strep throat), obesity, smoking, and even gut health are all suspected triggers. Research now shows that people with PsA have different gut bacteria than those without it. This "gut-skin-joint axis" theory suggests that imbalances in your microbiome might be fueling the immune system’s misfire.
At the molecular level, key inflammatory proteins like TNF-alpha, IL-17, and IL-23 are running wild. These are the same molecules targeted by modern treatments - and that’s why understanding them changed everything.
Treatment: From Pain Relief to Stopping the Damage
Treating PsA isn’t about masking pain. It’s about stopping the immune system from destroying your body. The goal? Minimal disease activity - a set of strict targets doctors use to measure success.That means:
- One or fewer tender or swollen joints
- Less than 1% of your skin covered in plaques
- Pain score under 15 out of 100
- Ability to do daily tasks without fatigue
Here’s how treatment usually unfolds:
- NSAIDs: For mild cases - ibuprofen or naproxen help with pain and swelling, but they don’t stop joint damage.
- DMARDs: Methotrexate (15-25 mg per week) is often the next step. It slows the immune system’s attack, but it’s not always enough for PsA.
- Biologics: These are targeted drugs that block specific inflammatory proteins. TNF inhibitors (like adalimumab and etanercept) are the most common. They work for about half of patients, with 30-40% seeing a 50% improvement in symptoms.
- IL-17 and IL-23 inhibitors: Drugs like secukinumab, ixekizumab, and guselkumab are better for skin symptoms and may work faster than TNF blockers. They’re now first-line for patients with severe psoriasis.
- JAK inhibitors: Tofacitinib is an oral option for those who can’t use injections or infusions.
Choosing the right drug depends on what’s hurting most. If your spine is stiff, TNF blockers are preferred. If your skin is flaring, IL-17 inhibitors win. And if you’ve tried multiple drugs without success, newer options like deucravacitinib (a TYK2 inhibitor) are showing promise in trials.
The Hidden Dangers: Comorbidities You Can’t Ignore
PsA isn’t just a skin and joint disease. It’s a whole-body condition. People with PsA have a 43% higher risk of heart attack. About half also have metabolic syndrome - high blood pressure, high blood sugar, excess belly fat, and abnormal cholesterol. That’s not a coincidence. Chronic inflammation drives all of it.Depression and anxiety affect 20-30% of PsA patients. When you’re in constant pain, your skin is visible and embarrassing, and your joints won’t let you play with your kids or hike on weekends, it takes a toll. Studies show quality of life scores are 30-40% lower than in healthy people your age.
And here’s the scariest part: mortality is 30-50% higher in PsA patients than in the general population - mostly because of heart disease. That’s why treatment isn’t just about joints and skin. Your doctor should be checking your blood pressure, cholesterol, and blood sugar. You need to move more, eat better, and quit smoking - not because it’s "good advice," but because it’s part of your treatment plan.
What’s Next? The Future of PsA Care
By 2027, experts predict 70% of PsA patients will be on biologics or targeted drugs within two years of diagnosis. That’s up from just 40% today. Why? Because we now know that early, aggressive treatment prevents permanent joint damage.New research is looking at blood biomarkers - like calprotectin and MMP-3 - to predict who will get severe PsA and who will respond best to which drug. That’s precision medicine in action: not trial and error, but the right drug for your body.
Ultrasound and MRI are getting better at spotting inflammation before it shows on X-rays. Clinical trials are testing drugs that target two pathways at once, like bimekizumab, which blocks both IL-17A and IL-17F. And studies on the gut microbiome might lead to probiotics or dietary changes as part of treatment.
One thing’s clear: PsA is no longer a sentence. It’s a manageable condition - if you catch it early and treat it fully.
What Should You Do If You Suspect PsA?
If you have psoriasis and notice any of these:- Swollen fingers or toes
- Stiffness in your back or neck that lasts more than 30 minutes in the morning
- Heel pain that doesn’t go away
- Nail changes you’ve never had before
Don’t wait. See a rheumatologist. Bring your dermatologist’s notes. Ask for a joint exam and imaging. Don’t let anyone tell you it’s "just aging" or "overuse." This is an autoimmune disease - and it needs a specialist.
And if you’ve been diagnosed: stay on your treatment. Even if your skin looks better, your joints might still be under attack. Keep your appointments. Track your symptoms. Push for the goal of minimal disease activity - not just "less pain."
PsA doesn’t have to steal your life. But you have to fight for your health - and you’re not alone.
Can psoriasis turn into psoriatic arthritis?
Not exactly. Psoriasis doesn’t "turn into" psoriatic arthritis. Both are caused by the same underlying autoimmune process. About 30% of people with psoriasis will develop joint symptoms - but the skin and joint problems happen at the same time, not one changing into the other. It’s one disease with two main expressions.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. While both cause joint swelling and pain, they’re different diseases. Rheumatoid arthritis usually affects joints symmetrically (both hands, both knees) and is linked to rheumatoid factor in the blood. Psoriatic arthritis often affects joints unevenly, causes dactylitis and enthesitis, and is linked to psoriasis and nail changes. Blood tests for rheumatoid factor are negative in most PsA cases.
Can you have psoriatic arthritis without skin psoriasis?
Yes - but it’s rare. About 5-10% of people develop joint symptoms before any skin rash appears. In those cases, doctors look for a family history of psoriasis, nail changes, or subtle skin signs like scalp scaling. Many will develop skin plaques later, even if they’re not visible at first.
Does stress cause psoriatic arthritis?
Stress doesn’t cause PsA, but it can trigger flares. If you already have the autoimmune condition, emotional stress, illness, or injury can make symptoms worse. Managing stress through sleep, exercise, or therapy can help reduce flare frequency - but it won’t prevent the disease from developing.
Are biologics safe for long-term use?
Biologics are generally safe for long-term use when monitored. They suppress part of the immune system, so there’s a small increased risk of infections like tuberculosis or fungal infections. That’s why doctors screen for latent infections before starting treatment. Regular blood tests and check-ups help catch issues early. For most people, the benefits - stopping joint damage and improving quality of life - far outweigh the risks.
Can diet cure psoriatic arthritis?
No diet can cure PsA. But losing weight if you’re overweight can significantly reduce symptoms - fat tissue produces inflammatory chemicals. Some people find that cutting out alcohol, sugar, or processed foods helps with inflammation. The Mediterranean diet, rich in fish, vegetables, and olive oil, is often recommended. But diet alone won’t replace medication. It’s a support tool, not a cure.


Conor McNamara
so u know they’re hiding the real cause right? it’s not genetics or gut bugs… it’s 5g radiation + chemtrails messing with your mitochondria. i’ve been tracking this since 2018. dermatologists won’t tell you because they’re paid by big pharma. my cousin had psoriasis for 12 yrs, stopped using his phone, ate only raw garlic, and it vanished. no meds. no biologics. just truth.
Leilani O'Neill
How quaint. The Irish healthcare system is still stuck in the 20th century while Germany and Switzerland have already moved to precision immunomodulation based on HLA haplotype and microbiome sequencing. You people think NSAIDs and methotrexate are treatment? This is why your life expectancy for autoimmune patients lags behind the EU average. Wake up.
Riohlo (Or Rio) Marie
Let’s be real - the entire medical industrial complex is just repackaging inflammation as a ‘disease’ so they can sell you $12,000-a-year biologics. The real solution? Stop eating gluten, stop drinking wine, stop pretending you’re ‘stressed’ when you’re just emotionally lazy. My cousin’s rheumatologist in Berlin told her to quit her job, move to the Alps, and hug trees for 40 minutes daily. She’s been in remission for 5 years. No drugs. Just radical life recalibration. The system doesn’t want you to know this works.
steffi walsh
Just wanted to say - if you’re reading this and feeling overwhelmed, you’re not alone. I was diagnosed 3 years ago with PsA and thought my life was over. Now I do yoga, track my sleep, and take my biologic religiously. Some days are rough, but I can hold my niece’s hand again. You’ve got this. 💪❤️
Gabe Solack
Great breakdown. One thing I’d add - don’t ignore your mental health. I had PsA for 5 years before I realized my anxiety was making the flares worse. Therapy + a daily walk made more difference than I expected. Also, if your doc won’t order an MRI, find a new one. Early detection = less damage. 🙌
Yash Nair
all this western medicine is garbage. in india we use turmeric paste, neem leaves, and sunbathing. no drugs needed. why are you letting pharma poison you? my uncle had psoriasis since 1980 and never took a pill. just ate ghee and chanted om. cured. you guys are weak.
Bailey Sheppard
Thanks for writing this. I’ve had psoriasis since I was 16 and just got diagnosed with PsA last year. It’s scary, but knowing what to look for - like dactylitis and enthesitis - made me finally push for the right tests. I’m on secukinumab now. Skin’s 90% better. Joints still ache sometimes, but I’m not giving up. Keep pushing for care. You deserve it.
Louie Amour
Oh please. You think this is complicated? It’s simple: your immune system is weak because you’re a lazy, processed-food-eating, screen-addicted zombie. Stop blaming genes. Stop blaming 5G. Stop wasting money on biologics. Go outside. Lift weights. Eat real food. Sleep 8 hours. That’s it. No pills. No specialists. Just discipline. You’re not sick - you’re just pathetic.