Medication Interaction Checker
Check Your Medications
Enter medications you're taking (prescription, OTC, supplements, or foods) and we'll check for potential interactions.
Separate each item with a comma. Include dosages if known.
Every year, over a million people in the U.S. end up in the hospital because of medication errors - and nearly 7% of those are due to dangerous drug interactions. You might think your doctor has covered everything, but the truth is, pharmacists are the real experts when it comes to how your medicines work together. They don’t just hand out pills - they know which ones clash with grapefruit juice, which supplements cancel out your birth control, and why that antacid you take for heartburn could make your Hepatitis C treatment useless.
What Medications, Supplements, or Foods Should I Avoid?
This is the most basic but most overlooked question. Don’t just say, “Is this safe?” Ask specifically: What medications, supplements, or foods should I avoid while taking this? Many people don’t realize that over-the-counter painkillers like ibuprofen can increase bleeding risk when taken with blood thinners like warfarin. Or that St. John’s Wort - a popular herbal remedy for mood - can make antidepressants, birth control, and even heart medications stop working. A 2020 University of Utah Health study found that 37.4% of people on warfarin didn’t know cranberry juice could make them bleed more. That’s not fear-mongering - that’s a real, documented risk.Does This Medicine Interact With Anything I’m Already Taking?
Most people forget to tell their pharmacist about every pill they take. Not just prescriptions - but the daily aspirin, the magnesium supplement, the melatonin for sleep, the cough syrup from last winter. Pharmacists need the full picture. One patient on Reddit shared how their pharmacist caught that their levothyroxine (a thyroid med) was being blocked by their calcium supplement. The result? Their thyroid levels stayed unstable for months because they never mentioned the calcium. The fix? Take them four hours apart. Simple. But only a pharmacist would know that. Ask: “I’m taking X, Y, and Z. Will any of them interfere with this new one?”Can I Drink Alcohol With This?
Alcohol doesn’t just make you sleepy - it can turn a safe medication into a dangerous one. Metronidazole (an antibiotic) causes vomiting, rapid heartbeat, and flushing if mixed with alcohol. Even common meds like acetaminophen (Tylenol) can harm your liver if taken with regular drinking. The National Institute on Alcohol Abuse and Alcoholism says over 42% of adults take at least one medication that reacts badly with alcohol. Yet, most people don’t ask. Don’t assume it’s fine. Say: “Is it safe to have even one drink while on this?”Does This Medicine Interact With Grapefruit or Other Juices?
Grapefruit juice isn’t just a tasty breakfast addition - it’s a silent drug amplifier. It blocks an enzyme in your gut (CYP3A4) that normally breaks down certain medications. The result? Your body absorbs way more of the drug than intended. For statins like atorvastatin, grapefruit can spike blood levels by up to 1500%. That increases the risk of muscle damage and kidney failure. The FDA says grapefruit affects about 85 prescription drugs - including some blood pressure meds, anti-anxiety pills, and cholesterol drugs. If you like grapefruit, ask: “Is this one on the list?” And if you’re not sure, just skip it while you’re on the med.Will This Affect My Sun Exposure?
Some medications make your skin hypersensitive to sunlight. Tetracycline antibiotics, certain diuretics, and even some antidepressants can cause severe sunburns, rashes, or long-term skin discoloration. You might think you’re just getting a tan - but it could be a reaction. Dr. Erika Brown, a lead pharmacist in Wisconsin, says patients often don’t realize their skin changes are drug-related. Ask: “Will this make me burn easier or change my skin color in the sun?” Then plan accordingly - wear sunscreen, cover up, or avoid midday sun.
Do I Need Any Tests While Taking This?
Not all interactions show up as symptoms right away. Some slowly build up - like liver damage from statins or kidney stress from NSAIDs. Your pharmacist can tell you if your medication requires monitoring. For example, if you’re on warfarin, you’ll need regular INR blood tests. If you’re taking lithium, your kidney and thyroid levels need checking. Even newer medications like certain Hepatitis C drugs require liver enzyme tests. Ask: “Will I need blood work or other tests to make sure this is safe for me?” Don’t wait for your doctor to bring it up - be proactive.What Should I Do If I Miss a Dose?
This isn’t just about adherence - it’s about safety. Missing a dose of some meds can trigger rebound effects or dangerous spikes in blood pressure. For others, doubling up can cause overdose. For example, if you miss a dose of your blood thinner, taking two later might put you at risk for bleeding. But if you miss a dose of your birth control, doubling up won’t help - you’ll need backup protection. Ask: “What happens if I forget to take this? Should I skip it or double up?” And ask if timing matters - like taking levothyroxine on an empty stomach, 30 minutes before food.Could This Interact With My Chronic Condition?
If you have diabetes, heart disease, kidney problems, or liver issues, your body handles drugs differently. A medication that’s safe for a healthy person might be risky for you. For instance, NSAIDs like ibuprofen can worsen kidney function in people with chronic kidney disease. Antacids like Tums can interfere with how your body absorbs thyroid or iron meds. Your pharmacist knows which meds are risky for which conditions. Say: “I have [condition]. Is this medicine safe for me, given that?”Should I Be Watching for Any Warning Signs?
You don’t need to be a doctor to spot trouble. Learn what red flags to look for. Serotonin syndrome - from mixing SSRIs with certain migraine meds or supplements - can cause confusion, rapid heartbeat, muscle rigidity, and high fever. Disulfiram-like reactions from alcohol and antibiotics cause flushing, nausea, and chest pain. Muscle pain or weakness could signal statin toxicity. Ask your pharmacist: “What are the signs I should call you or go to the ER about?” Write them down. Keep them on your phone. It could save your life.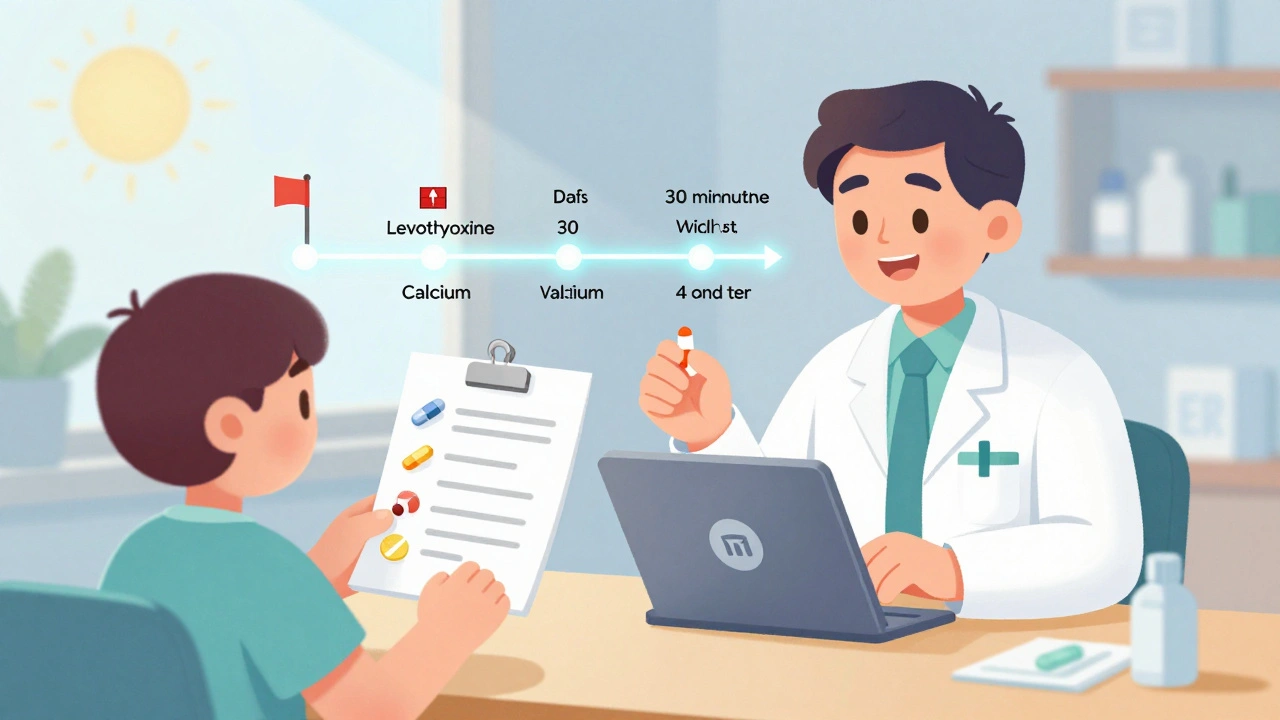


Karen Mccullouch
OMG I CANNOT BELIEVE PEOPLE DON’T ASK THIS!! 😤 I took ibuprofen with my blood thinner and almost ended up in the ER. My pharmacist had to yell at me through the drive-thru window. STOP BEING LAZY AND ASK!! 🚨
Michael Gardner
Funny how this post treats pharmacists like some kind of miracle workers. Meanwhile, I’ve had pharmacists give me wrong info because they were rushing, or didn’t even know what my supplement was. This is just corporate propaganda dressed up as helpful advice.
Willie Onst
Hey y’all, just wanted to say this is one of those posts that reminds me why I love this country. 🇺🇸 People are finally waking up to the fact that we’re not just passive patients-we’re partners in our own health. I used to think my pharmacist was just a pill dispenser, but after I asked about grapefruit and my statin? He gave me a pamphlet, a hug, and a free sample of generic fish oil. That’s the kind of care we need more of. Keep asking. Keep caring. You’re not being annoying-you’re being human.
Jennifer Taylor
I KNOW WHAT YOU’RE NOT TELLING ME. 🕵️♀️ They’re all in on it. Big Pharma pays pharmacists to NOT tell you about interactions because if you knew how many meds cancel each other out, you’d stop taking everything. I’ve been tracking my pills since 2018 and I swear my thyroid med turns into a placebo after 3 weeks. They don’t want you to know the truth. 🧪 #PharmaCoverup #GrapefruitIsASpy
Shelby Ume
I appreciate this thoughtful breakdown. As a nurse who works closely with pharmacists, I can confirm that the most effective patients are the ones who come in with a printed list-dated, annotated, and updated. It’s not just about safety; it’s about dignity. You deserve to understand what’s in your body. And yes, even that ‘natural’ turmeric capsule? Write it down. I’ve seen too many patients with liver enzymes through the roof because they thought ‘herbal’ meant ‘harmless.’ You’re not being difficult-you’re being responsible.
Jade Hovet
i literally just asked my pharmacist about my melatonin + blood pressure med and she was like ‘ohhhhh that’s why your bp was spiking!’ 😭 thank u for this post!! i started using mytherapy app and it’s a game changer. also, i always forget to write down my gummy vitamins… but now i do! 🙌❤️ #pharmacistlove #medsafety
nina nakamura
You people are idiots. The real problem isn’t that you don’t ask questions-it’s that you’re too lazy to read the damn patient info leaflet. Every single interaction listed here is in the pamphlet that comes with your pill bottle. If you can’t read, get glasses. If you won’t read, stop pretending you care. Your ignorance is a burden on the system.
Rawlson King
This is exactly why I moved to Canada. Here, pharmacists have time. They sit down. They ask about your diet, your sleep, your stress levels. In the U.S., you’re a number on a screen. You think asking questions is brave? It’s just survival. Americans have been conditioned to trust authority without question. That’s not wisdom-that’s programming.
Constantine Vigderman
Y’ALL I JUST GOT MY NEW PRESCRIPTION AND I ASKED ABOUT GRAPEFRUIT AND MY PHARMACIST SAID ‘OH YEAH THAT’S A BIG ONE’ AND THEN SHOWED ME A LITTLE CHART WITH ALL THE DRUGS IT AFFECTS 😍 I FEEL SO GOOD ABOUT MY HEALTH NOW. I’M GONNA TELL MY MOM TO DO THE SAME. WE GOT THIS!! 💪❤️ #pharmacisthero #askmore #medsafetyrock