When you’re prescribed a biologic drug - say, for rheumatoid arthritis, Crohn’s disease, or psoriasis - you might see a price tag of $80,000 a year. That’s not a typo. For many patients, that’s more than their annual rent. But what if there was a version of the same medicine that works just as well, costs less than half, and has been approved by the FDA as safe and effective? That’s where biosimilars come in.
What Exactly Is a Biosimilar?
You’ve heard of generic pills - the cheap versions of drugs like metformin or lisinopril. Those are simple chemicals made in labs. Biosimilars are different. They’re copies of biologic drugs, which are made from living cells - not chemicals. Think insulin, antibodies, or proteins grown in bioreactors. Because they come from living systems, no two batches are exactly alike. That’s why biosimilars aren’t called “generics.” They’re “highly similar,” with no clinically meaningful differences in safety or effectiveness. The FDA approved the first biosimilar, Zarxio, in 2015. Since then, 76 have been approved as of October 2025. That sounds like a lot - until you realize there are about 600 biologics on the market. Most still have no competition.How Much Do Biosimilars Save?
The numbers don’t lie. In the first half of 2025, the average 30-day cost for a brand biologic was $2,104. The biosimilar version? $919. That’s a 56.3% drop. For a patient on monthly injections, that’s over $14,000 saved per year. Take Humira, the world’s best-selling drug for years. Before biosimilars hit the market, it cost about $80,000 per patient annually in the U.S. After patents expired in 2023, biosimilars entered with discounts averaging 80%. By mid-2025, they held 65% of the market. One biosimilar, Hyrimoz by Sandoz, captured 14% of sales on its own - and it costs less than $16,000 a year. Patients aren’t just saving on the drug price. Out-of-pocket costs - what you pay at the pharmacy - are 23% lower with biosimilars. That’s huge for people on high-deductible plans or without good insurance.Why Aren’t More People Using Them?
If biosimilars save so much money, why isn’t everyone switching? One reason: the system is rigged. Brand drug companies don’t just rely on patents - they build patent thickets. That means filing dozens of minor, overlapping patents to delay biosimilar entry. Some biologics have over 100 patents. Even after the main patent expires, legal battles can delay competition for years. Then there are Pharmacy Benefit Managers (PBMs). These middlemen negotiate rebates with drugmakers. But here’s the catch: they often get bigger rebates from expensive brand drugs than from cheaper biosimilars. So even if a biosimilar is cheaper, the PBM pushes the brand version because it pays them more. It’s not about saving money - it’s about who gets the kickback. Doctors and pharmacists also get confused. Many still think biosimilars are “less effective.” But the FDA says they’re not. A 2025 Harvard Medical School study found zero difference in outcomes between patients on brand biologics and those on biosimilars.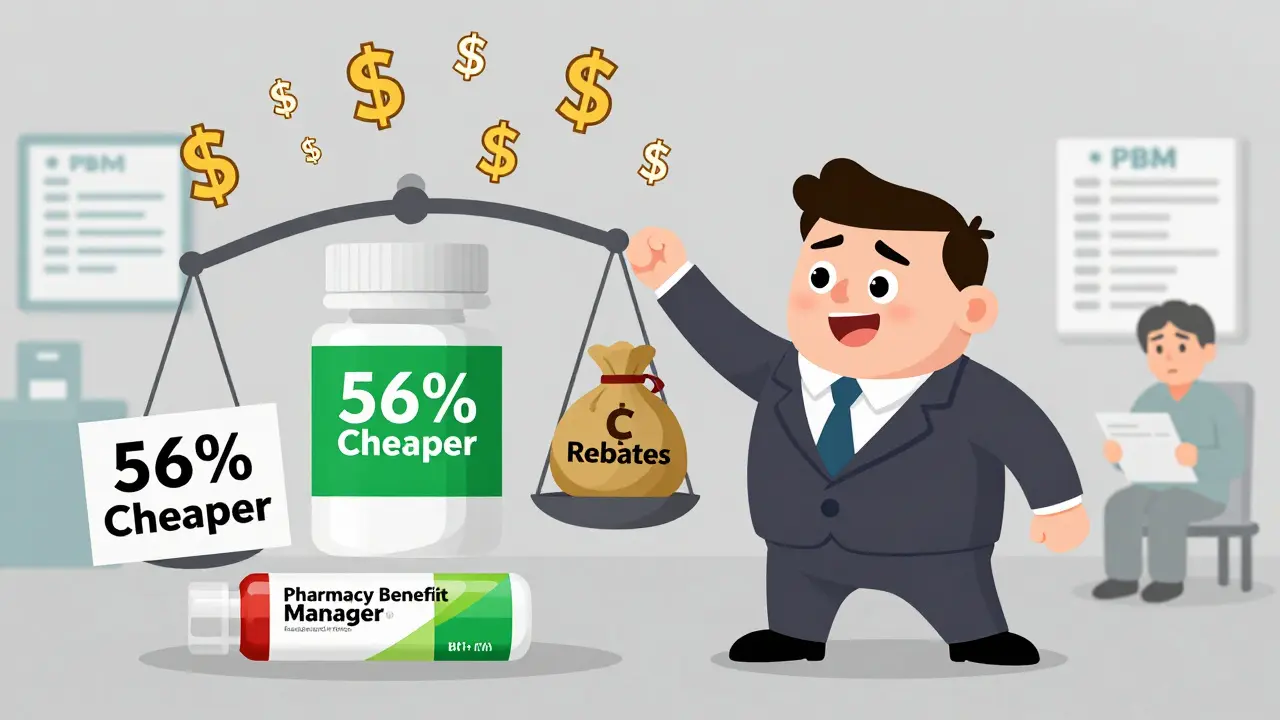
How Much Have Biosimilars Saved So Far?
The savings are massive - but different groups report different numbers. The U.S. Department of Health and Human Services says biosimilars have saved $56 billion since 2015, with $20 billion saved in 2024 alone. Other analysts, like DrugPatentWatch, estimate $36 billion total since 2015. Either way, that’s billions in savings for patients, insurers, and taxpayers. And it’s not just biosimilars. When a biosimilar enters the market, the brand drug often lowers its price too - by an average of 25%. That’s called the “spillover effect.” So even if you don’t switch, you still pay less. In 2023, all generic and biosimilar drugs combined saved the U.S. healthcare system $445 billion. That’s more than the entire annual budget of the Department of Education. And yet, generics and biosimilars make up 90% of all prescriptions - but only 13% of total drug spending.What’s Holding Back the Next Wave?
There are over 100 biologics expected to lose patent protection in the next 10 years. But only about 10% of them have a biosimilar in development. Why? Developing a biosimilar costs between $100 million and $250 million. That’s 10 times more than making a regular generic. It takes 7-10 years. And the approval process is still more complex than it needs to be. The FDA is trying to fix this. In September 2025, they released new draft guidelines to simplify testing and cut unnecessary clinical trials. That could shave years off development time and lower costs. The Biden administration’s Biosimilars Action Plan also aims to fix reimbursement rules so that doctors and pharmacies are rewarded for choosing cheaper options - not punished.
What’s the Future Look Like?
By 2030, biosimilar market share could jump from 15-20% to 35-40%. That could mean $125 billion in new annual savings - enough to cover free insulin for every diabetic in the U.S. for five years. But that future isn’t guaranteed. Without policy changes - like banning patent thickets, forcing PBMs to pass savings to patients, and creating clearer reimbursement rules - the savings will stay locked away. Right now, the U.S. spends more on drugs than any other country. And biologics are the biggest reason why. Biosimilars aren’t a magic fix - but they’re the most powerful tool we have to bring prices down without sacrificing care.What Should You Do?
If you’re on a biologic drug:- Ask your doctor if a biosimilar is available and appropriate for you.
- Check your insurance formulary - some plans cover biosimilars at lower copays.
- Don’t assume your current drug is the only option. Many patients switch without any loss in effectiveness.
- Use tools like GoodRx or NeedyMeds to compare prices. Biosimilars often cost less even before insurance.


Dave Alponvyr
So the system literally pays pharmacies to push expensive drugs? That’s not broken-it’s designed that way.
Cassandra Collins
Wait… so PBMs are the real villains? And the FDA’s just playing along? I swear I read somewhere that Big Pharma owns half the congress. This isn’t about drugs-it’s about control. They don’t want you healthy, they want you hooked.
Kim Hines
I switched to a biosimilar for my psoriasis last year. No difference. My skin’s fine. My bank account is too.
Souhardya Paul
Really appreciate this breakdown. I didn’t realize how much of the cost gap comes from PBM rebates rather than actual drug pricing. It’s wild how the incentive structure rewards the most expensive option-even when it’s not better. I’ve been telling my rheumatologist about biosimilars for months, and she finally agreed to switch me after I showed her the 2025 Harvard data. No side effects, same results. If more docs knew this, we’d see way more adoption.
Also, the spillover effect is huge. My Humira copay dropped from $450 to $280 just because Hyrimoz came out. I didn’t even switch, but I still saved $2k/year. That’s the real win.
Hadi Santoso
As someone who moved from Indonesia to the US, I can’t believe how insane drug prices are here. Back home, insulin costs like $10 a month. Biosimilars? Totally normal. Here, people are choosing between rent and their meds. And the worst part? Everyone acts like it’s just how things are. It’s not. It’s politics. And it’s cruel.
Also, typo: ‘Hyrimoz’ not ‘Hyrimoz’ - just sayin’ 😅
Joanna Ebizie
Ugh stop pretending biosimilars are safe. My cousin took one and got hospitalized with a rash. The FDA approves stuff based on paperwork, not real people. You think they care if you live or die? They’re making billions off this. Don’t be a guinea pig.
Arun ana
From India, where generics are cheap and everywhere. Biosimilars here? We’ve had them for 10+ years. Price? $100/year for Humira copy. No drama. No lawsuits. Just medicine. Why is the US so slow? Is it because we don’t have lobbyists with private jets?
Also, emoji for the win 🤷♂️
Dylan Smith
It’s not even close to being about science anymore. It’s about who owns the patents and who gets the kickbacks. The fact that a $16k biosimilar can take 65% of the market and still be considered a ‘success’ means the original $80k drug was always a scam. They knew people would pay it. They planned it. And now they’re trying to delay the next wave with 100-patent thickets. This isn’t innovation-it’s extortion.
The Biden plan is a start but it’s toothless without banning rebate structures. PBMs need to be forced to pass savings to patients. Not just ‘disclose.’ Not just ‘try.’ FORCE IT. Or shut them down.
And doctors? Stop being lazy. If you’re not asking your patients about biosimilars every time you write a script, you’re part of the problem. It’s not hard. It’s not risky. It’s just cheaper. And you know it.
Elizabeth Bauman
Look, I get it. Biosimilars save money. But let’s not pretend the U.S. is the only country with drug problems. Europe has price controls. Canada has single-payer. China has state-run pharma. We’re a free market. If you can’t afford your medicine, maybe you shouldn’t be on it. Or maybe you should move to a country that gives you free stuff. This isn’t entitlement-it’s responsibility.
Also, I’ve seen the data. The FDA doesn’t approve junk. If they say it’s safe, it’s safe. Stop the fearmongering. We don’t need conspiracy theories-we need personal accountability.
Mike Smith
Thank you for this comprehensive and well-researched analysis. The systemic barriers to biosimilar adoption are not merely logistical-they are deeply structural, rooted in financial incentives that misalign clinical outcomes with economic efficiency. The FDA’s recent draft guidelines represent a meaningful step toward reducing development burdens, but legislative intervention is imperative to dismantle patent thickets and reform PBM rebate structures. Without mandating pass-through savings to patients and incentivizing provider adoption through transparent reimbursement models, the potential for $125 billion in annual savings will remain unrealized. This is not a pharmaceutical issue-it is a public health imperative.
Souhardya Paul
Mike, you nailed it. The PBM rebate system is the real cancer here. I talked to my insurance rep last week-they admitted they get 3x the rebate on the brand vs. the biosimilar. So even though Hyrimoz is cheaper, they still push Humira because it pays them more. That’s not a mistake. That’s the business model. And it’s why we need laws that force transparency and ban these kickbacks. No more ‘negotiated rebates’ that never reach patients. Just straight-up price caps and mandatory pass-throughs.
Also, Elizabeth-your point about personal responsibility is valid, but here’s the thing: people don’t choose to get rheumatoid arthritis or Crohn’s. They don’t choose to need biologics. And if the system makes it impossible to afford life-saving care, then the system is the problem, not the patient.