Urticaria-commonly called hives-is more than just a rash. It’s a sudden, itchy, raised welt that can appear anywhere on your skin, often without warning. One moment you’re fine; the next, your arm or neck is covered in red, swollen bumps that burn and itch like crazy. For some, it lasts a few hours. For others, it comes back every day for months or even years. This isn’t just a nuisance-it can wreck sleep, ruin your mood, and make you feel like your body is working against you.
What causes it? Mostly, it’s histamine. Your body’s immune system releases this chemical in response to something it thinks is a threat-even when there’s no real danger. That histamine leaks fluid into your skin, creating those telltale welts. The good news? Most cases respond well to simple, over-the-counter meds. The tricky part? Figuring out what’s triggering it in the first place.
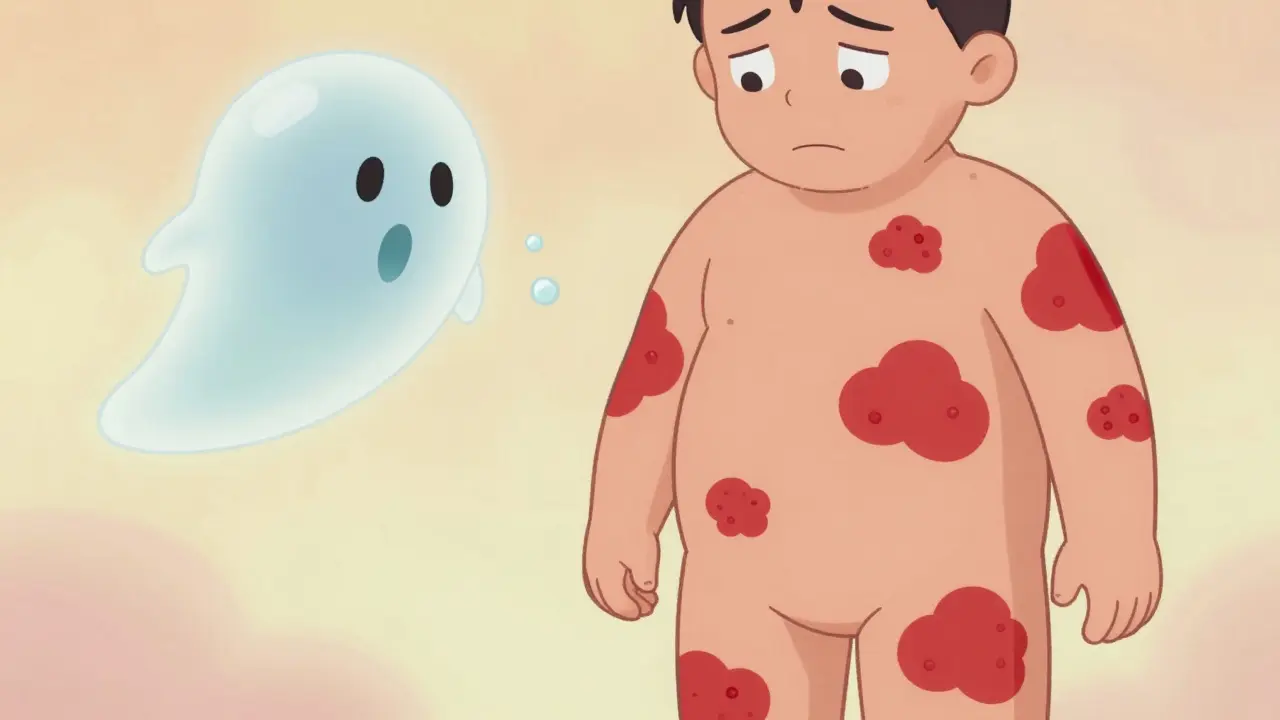
What Do Hives Actually Look Like?
Hives aren’t one-size-fits-all. They can be tiny spots the size of a pencil eraser or merge into large, angry patches that cover your whole back. They’re usually red or pink, with a pale center, and they shift shape and location fast. A welt might show up on your thigh at 9 a.m., disappear by noon, then reappear on your forearm by 4 p.m. That’s normal. If a welt lasts longer than 24 hours in the same spot, it’s probably not hives-it could be something else, like vasculitis or an infection.
There are two main types: acute and chronic. Acute urticaria lasts less than six weeks. It often follows something clear-a new food, a bee sting, antibiotics, or a viral infection like a cold. Chronic urticaria lasts six weeks or longer. About 70-80% of chronic cases have no obvious trigger. Doctors call this chronic spontaneous urticaria. It’s frustrating because you can’t just avoid the trigger-you don’t know what it is.
What Triggers Hives? Not Just Allergies
Most people assume hives mean an allergy. But only about 10-20% of cases are true allergic reactions. The rest? They’re triggered by things you wouldn’t expect.
- Physical triggers: Cold, heat, sweat, pressure, sunlight, or even scratching your skin (called dermographism). If you get hives after a cold shower or when your belt digs into your waist, you’ve got a physical form.
- Infections: Viral infections (like hepatitis or Epstein-Barr), bacterial infections (like strep throat), or even parasites can set off hives.
- Medications: NSAIDs like ibuprofen or aspirin, antibiotics like penicillin, and even some blood pressure meds can cause reactions.
- Stress: Emotional stress doesn’t cause hives directly, but it can make them worse. Studies show stress hormones can increase histamine release.
- AUTOIMMUNE: In 30-40% of chronic cases, your body makes antibodies that attack your own mast cells-the very cells that release histamine. This isn’t an allergy. It’s your immune system turning on itself.
That’s why keeping a daily symptom diary matters. Note what you ate, what you touched, how stressed you felt, even your sleep quality. Many patients find patterns after 2-4 weeks of tracking. Apps like Urticaria Tracker help, but a simple notebook works too.
Antihistamines: The First Line of Defense
If you’ve got hives, your doctor will almost always start you on an antihistamine. These drugs block histamine from binding to receptors in your skin, reducing swelling, redness, and itch. But not all antihistamines are the same.
Second-generation antihistamines are the gold standard. They’re non-drowsy, last 24 hours, and have fewer side effects. These include:
- Cetirizine (Zyrtec): 10mg daily. Works fast-often within an hour. About 60% of users report good relief.
- Loratadine (Claritin): 10mg daily. Less effective for some. One user wrote: "It works for 4-6 hours, then I’m back to scratching."
- Fexofenadine (Allegra): 180mg daily. Lowest drowsiness risk. Scores 4.1/5 in effectiveness ratings.
First-generation antihistamines like diphenhydramine (Benadryl) work fast but make 50-70% of people drowsy. They’re useful for nighttime relief but not for daily use during the day. Many patients use a combo: a non-drowsy one in the morning, and a sedating one at night if itching keeps them awake.
Here’s the twist: For chronic hives, standard doses often aren’t enough. The 2023 international guidelines say you can safely increase the dose up to 4 times the normal amount. So if 10mg of cetirizine isn’t working, try 20mg. Many patients see big improvements-up to 50% more symptom control-without serious side effects.
When Antihistamines Aren’t Enough
Half of chronic hives patients don’t get full relief from even high-dose antihistamines. That’s where things get more complex.
Omalizumab (Xolair) was the first biologic approved for chronic hives in 2014. It’s an injection given every 4 weeks under the skin. It targets IgE antibodies-those involved in allergic reactions. In clinical trials, 65% of patients who didn’t respond to antihistamines saw major improvement. On PatientsLikeMe, 72% of users reported satisfaction. But it costs about $1,500 per dose in the U.S., and not all insurance covers it.
In September 2023, the FDA approved dupilumab (Dupixent) for chronic hives. Originally for eczema and asthma, it’s now shown to give complete symptom relief in 55% of patients-double the placebo rate. It’s also an injection, given every two weeks.
Then came remibrutinib, approved in January 2024. This is the first oral tyrosine kinase inhibitor for hives. No shots. Just a pill, twice a day. In trials, 45% of patients had complete symptom control. It’s cheaper than biologics, and adherence is higher-85% of patients took it as prescribed vs. 70% for injections. It’s not yet widely available, but it’s a game-changer for people who hate needles.
Other options? Steroids like prednisone work fast, but they’re not for long-term use. After just 3-5 days, side effects kick in: insomnia, mood swings, high blood sugar. Cyclosporine helps too, but it can damage kidneys or raise blood pressure. These are last-resort options, used only when other treatments fail.
What About Natural Remedies?
You’ll see ads for quercetin, vitamin C, or nettle tea as "natural antihistamines." There’s no solid evidence they work for hives. Some small studies show mild benefit, but nothing compared to FDA-approved drugs. And if you’re on other meds, supplements can interact dangerously. Don’t swap proven treatments for unproven ones.
What does help? Avoiding known triggers. If heat makes your hives worse, skip hot showers. If pressure from your bra causes welts, try a soft, wire-free style. If stress spikes your symptoms, find a calming routine-breathing exercises, walking, even journaling. These won’t cure hives, but they can reduce flare-ups.

Living With Chronic Hives
It’s not just the itching. A Reddit survey of over 1,200 people with chronic hives found 68% said it disrupted their sleep. 42% woke up 2-3 times a night. 22% had to see three or more doctors before getting the right diagnosis. Many report anxiety, depression, or social isolation because they’re embarrassed by their skin.
Support matters. Groups like the Urticaria Patients Association connect people globally. Online communities offer practical tips: "I use cold compresses and loose cotton clothes," or "I keep my bedroom at 65°F to avoid night flares."
And yes-hives can get better. About 50% of chronic cases resolve within a year. Another 30% improve significantly with the right treatment. The key is persistence. Don’t give up if the first antihistamine doesn’t work. Try a higher dose. Talk to an allergist. Ask about biologics. You’re not alone.
When to See a Doctor
See a doctor if:
- Hives last more than 2 weeks
- You have swelling of the lips, tongue, or throat (angioedema)
- You feel dizzy, short of breath, or your heart races
- Over-the-counter meds don’t help after 3-5 days
These could signal a more serious reaction. If you’re having trouble breathing, call emergency services immediately.
Are hives contagious?
No, hives are not contagious. They’re caused by your body’s internal reaction to triggers-not by bacteria or viruses you can pass to someone else. You can’t catch hives from touching someone who has them.
Can stress cause hives?
Stress doesn’t directly cause hives, but it can make them worse. When you’re stressed, your body releases chemicals that boost histamine production. If you already have chronic hives, stress can trigger flares or make itching feel more intense. Managing stress through sleep, exercise, or mindfulness can help reduce frequency.
Why do antihistamines stop working over time?
Antihistamines don’t usually stop working-they just might not be strong enough. Many people with chronic hives need higher-than-standard doses. The body doesn’t build tolerance to antihistamines like it does to some other drugs. If your current dose isn’t helping, talk to your doctor about increasing it before switching meds.
Is there a cure for chronic hives?
There’s no guaranteed cure, but many people go into remission. About half of chronic hives cases resolve on their own within a year. For others, treatments like omalizumab, dupilumab, or remibrutinib can bring symptoms under full control. The goal isn’t always a cure-it’s managing symptoms so they don’t control your life.
Can I take antihistamines every day for years?
Yes. Second-generation antihistamines like cetirizine and fexofenadine are safe for long-term daily use. Studies have tracked patients on these meds for over 10 years with no major safety concerns. The real risk isn’t the drug-it’s leaving hives untreated, which affects sleep, mental health, and daily function.
Do I need allergy testing for hives?
Not always. For acute hives, especially after eating a new food or taking a new drug, testing can help. But for chronic spontaneous urticaria-which makes up most cases-allergy tests usually come back negative. That’s because the trigger isn’t an external allergen. It’s often internal, like an autoimmune reaction. Your doctor will focus more on symptom patterns and treatment response than on allergy tests.

Joe Grushkin
Hives aren't allergies. That's the first thing they get wrong. It's not your body being allergic to shrimp or pollen-it's your immune system throwing a tantrum because it's bored. We've turned medicine into a guessing game where the diagnosis is 'probably histamine' and the treatment is 'take this pill until it works or doesn't.' The real issue? We don't understand the immune system. We just throw drugs at it and call it science.
And don't get me started on 'natural remedies.' Quercetin? Nettle tea? Please. That's what people use when they can't afford real medicine or refuse to admit their body is broken. This isn't a yoga retreat. It's an autoimmune malfunction. Treat it like one.
They mention omalizumab and dupilumab like they're miracle cures. They're not. They're expensive Band-Aids for a system that's falling apart. And remibrutinib? A pill? Finally. But it took 10 years and $2 billion in R&D to get here. We're still treating symptoms like they're the disease.
Chronic hives aren't about triggers. They're about dysregulation. The body doesn't need to 'avoid stress' or 'wear loose clothes.' It needs a reset. We need to stop asking 'what triggered it' and start asking 'why is it still firing?'
The fact that 70% of chronic cases have no identifiable trigger isn't a mystery-it's a failure. We're diagnosing with a flashlight in a blackout. And patients? They're the ones left stumbling around in the dark, scratching their skin raw while doctors shrug and hand them another Zyrtec.
Virginia Kimball
Y’all need to hear this: you’re not broken. Seriously. I had hives for 14 months. Thought I was dying. Thought I was crazy. Went to five doctors. Got told to ‘relax’ and ‘drink more water.’
Then I tried doubling my cetirizine. Just doubled it. No doctor approval. Just read the guidelines. And boom-70% less itching. I could sleep. I could leave the house. I could stop crying in the shower.
It’s not about being ‘fixed.’ It’s about finding what works for YOUR body. Some people need the pill. Some need the cold compress. Some need to stop wearing bras with underwire. (Yes, that’s a real trigger.)
You’re not alone. I’ve talked to people from Tokyo to Toronto who are doing the same thing: tracking, tweaking, surviving. You’ve got this. One day at a time. One dose at a time. You’re not failing-you’re figuring it out.
Michael Page
The real tragedy isn’t the hives. It’s the medical system’s refusal to accept that some diseases don’t have clean answers. We want a trigger, a label, a pill. But chronic urticaria? It’s a whisper in a hurricane. A flicker in the dark.
Antihistamines work because they mute the signal-not because they fix the source. We treat the symptom like it’s the cause. We’re not curing. We’re managing. And that’s fine. But we pretend it’s something else.
The autoimmune component-30-40% of cases-isn’t a footnote. It’s the core. We should be researching mast cell autoimmunity like we do lupus or MS. But we don’t. Because it doesn’t have a sexy name. Because it doesn’t have a viral video.
Remibrutinib? A step. Not a solution. The real breakthrough will come when we stop asking ‘what’s wrong with you?’ and start asking ‘why is your immune system at war with itself?’
And until then? We’re all just scratching in the dark.
Josiah Demara
Let’s cut through the fluff. This post reads like a pharmaceutical brochure with a side of pseudoscience.
You say ‘stress doesn’t cause hives’-but then you say ‘stress makes them worse.’ That’s not nuance. That’s hand-waving. If stress modulates histamine release via cortisol and norepinephrine pathways-which it does-then yes, it’s a biological trigger. Stop pretending it’s not.
And ‘natural remedies’? Of course they’re not FDA-approved. They’re not patentable. So of course Big Pharma doesn’t fund them. But that doesn’t mean they’re useless. You’re acting like science only exists in pill form.
Also, ‘4x dose of antihistamines’? That’s not ‘safe.’ It’s ‘unregulated.’ You’re telling people to self-medicate with higher doses because the system failed them. That’s not advice. That’s negligence dressed up as empowerment.
And don’t get me started on biologics. Omalizumab costs $1,500 per shot? That’s not healthcare. That’s a luxury for the insured. The fact that this is even a conversation shows how broken this system is.
You didn’t explain hives. You sold a product list.
Charlotte Dacre
So let me get this straight-you’re telling me I’ve been wearing the wrong bra for three years and that’s why I look like I got into a fight with a swarm of bees? Brilliant.
Also, ‘don’t swap proven treatments for unproven ones’? Cool. Then why is every Reddit thread about hives full of people trying CBD oil, apple cider vinegar, and cold showers like it’s a cult initiation? You just gave them a textbook. Now they’re gonna treat it like a TikTok trend.
And remibrutinib? A pill? Finally. Took long enough. I’m just glad we’re moving from ‘inject yourself monthly’ to ‘swallow this like a vitamin.’ Progress. Slow, expensive, but progress.
Esha Pathak
When I first got hives, I thought it was karma for eating too much junk food. Then I realized-it’s not punishment. It’s communication.
My body was screaming, ‘Something’s off!’ But no one listened. Doctors said ‘stress.’ Friends said ‘allergy.’ I tried everything-tea, oils, fasting, crystals (yes, really).
Then I read about the autoimmune link. And I cried. Not because I was scared. But because for the first time, someone said: ‘This isn’t your fault.’
Now I take 20mg of cetirizine. I wear cotton. I meditate. I don’t chase triggers. I listen.
It’s not about curing. It’s about becoming friends with your body again. It’s not broken. It’s trying to tell you something.
And yes-I still get flares. But now I don’t hate my skin. I protect it.
Mike Hammer
man i had hives for like 8 months and i thought i was gonna die
turned out my laundry detergent was the culprit. like, the same one i’d been using since college
switched to free & clear and boom-gone in 3 days
so yeah maybe it’s not always autoimmune
sometimes it’s just… your soap
Daniel Dover
High-dose antihistamines work. I’ve seen it. No drama. Just science.
Chiruvella Pardha Krishna
The body doesn’t malfunction. It adapts. Hives aren’t a disease. They’re a language.
We call them ‘itchy welts’ because we fear what we can’t name. But what if they’re not errors? What if they’re signals-ancient, biological, screaming through histamine to say: ‘You are not safe.’
Stress. Toxins. Sleep. Trauma. These aren’t triggers. They’re conversations. And we’ve been too busy prescribing pills to listen.
Remibrutinib will help some. But the real cure? When we stop treating the skin-and start healing the silence.