When women start thinking about hormone therapy for menopause symptoms, the options can feel overwhelming. It’s not just about taking a pill-it’s about choosing the right hormone therapy combination for your body, your history, and your life. The good news? There are proven, affordable generic options that work well for most women. The catch? Picking the wrong one can increase risks you didn’t even know about.
Why Combination Therapy Matters
If you still have your uterus, you can’t take estrogen alone. It’s that simple. Estrogen makes the lining of your uterus grow. Left unchecked, that growth can turn into cancer. That’s why every woman with a uterus who takes estrogen also needs progestogen-either as a pill, an IUD, or in a combined patch. This isn’t optional. It’s medical safety. For women who’ve had a hysterectomy, estrogen-only therapy is safe and often preferred. It avoids the side effects of progestogen-like bloating, mood swings, and breakthrough bleeding-while still relieving hot flashes, night sweats, and vaginal dryness.Two Main Types of Combination Therapy
There are two ways to combine estrogen and progestogen, and which one you need depends on whether you’re still having periods.- Sequential combined HRT: This is for women in perimenopause or those who’ve had a period in the last year. You take estrogen every day, then add progestogen for 10-14 days each month. This mimics a natural cycle and usually causes a monthly bleed. It’s designed for women whose bodies are still adjusting to hormonal shifts.
- Continuous combined HRT: Once you’ve gone a full year without a period, this is the standard. You take both hormones every single day, with no breaks. No monthly bleeding. This is the go-to for most postmenopausal women.
The difference isn’t just timing-it’s safety. Continuous therapy lowers your risk of colon cancer by about 18% and type 2 diabetes by 21%, based on long-term data from the Women’s Health Initiative. But it also means you need to be sure you’re truly postmenopausal before switching.
Generic Hormones You Can Actually Trust
You don’t need brand-name products to get effective relief. Generic versions of estrogen and progestogen are widely available, well-tested, and cost a fraction of the branded options.- Estrogen: Conjugated estrogens (like Premarin generics) come in 0.3mg, 0.45mg, and 0.625mg tablets. Estradiol (like Estrace generics) is available in 0.5mg and 1mg. Estradiol is often preferred because it’s chemically identical to what your body makes.
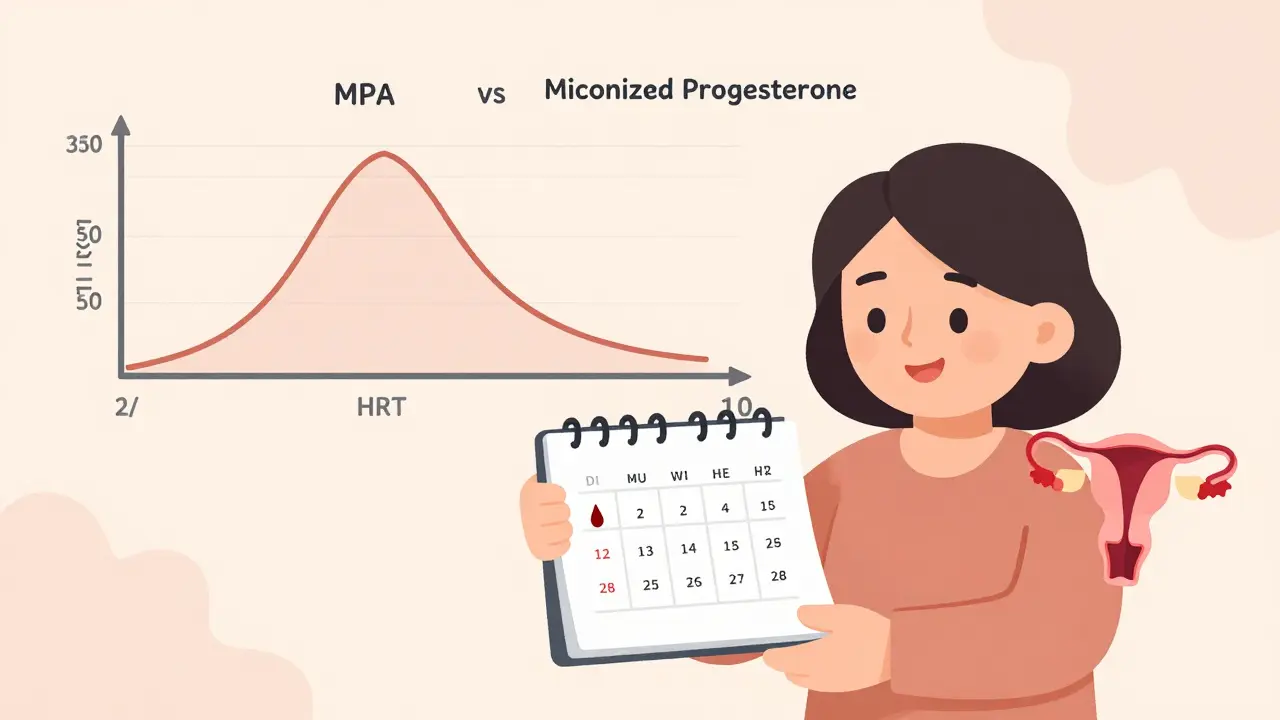
- Progestogen: Medroxyprogesterone acetate (MPA) is the most common generic progestogen, in 2.5mg, 5mg, and 10mg doses. Micronized progesterone (Prometrium) is also available generically and is considered safer for breast health.
Prices vary, but in the U.S., these generics typically cost between $4 and $40 a month, depending on your insurance and pharmacy. Many are covered at $10 or less through Walmart, CVS, or Costco’s generic programs.
Delivery Method Changes Everything
How you take your hormones matters more than you think. Oral pills aren’t the only-or even the safest-option.- Oral tablets: These are absorbed through your gut and processed by your liver. That’s why they raise your risk of blood clots by 2-3 times compared to other forms. The absolute risk is still low for healthy women under 60, but it’s real.
- Transdermal patches, gels, sprays: These deliver hormones directly through your skin, skipping the liver. That means far less impact on clotting factors. The risk of venous thromboembolism (VTE) drops by about 60% compared to pills. If you have a history of clots, high blood pressure, or are over 60, this is your best bet.
- Intrauterine systems (IUS): The Mirena coil releases progestogen directly into the uterus. It’s perfect for women who want to reduce bleeding and protect the uterine lining without taking daily pills. Many women use it with a transdermal estrogen patch for full protection.
Europeans use transdermal options 65% of the time. In the U.S., it’s only 35%. But that’s changing. More doctors are starting with patches or gels, especially for women over 50.
Breast Cancer Risk: What the Data Really Says
The fear of breast cancer is one of the biggest reasons women avoid hormone therapy. But the numbers need context.- Combined HRT (estrogen + progestogen) slightly increases breast cancer risk after 5+ years of use. The Cleveland Clinic estimates less than 1 in 1,000 women per year will develop breast cancer because of it.
- Synthetic progestins like MPA raise risk by 2.7% per year of use.
- Micronized progesterone (natural progesterone) raises it by only 1.9% per year.
That’s a meaningful difference. If you’re planning to use HRT for more than 3-5 years, choosing micronized progesterone over MPA can reduce your breast cancer risk by nearly 30% over time. It’s not just a preference-it’s a smart choice.
When Hormone Therapy Isn’t Safe
HRT isn’t for everyone. It’s not a fountain of youth. It’s a symptom treatment.- Avoid oral HRT if you’re over 60, have a history of stroke, blood clots, or heart disease. Transdermal estrogen is safer here, but even then, start low and go slow.
- Don’t use HRT to prevent heart disease, dementia, or osteoporosis. The evidence doesn’t support it. There are better, safer ways.
- If you’ve had estrogen-sensitive breast cancer, HRT is generally contraindicated. Talk to your oncologist first.
Dr. Gutierrez at Houston Methodist puts it bluntly: “Throwing hormones at an older woman with a history of heart disease can be very harmful.” Timing and health status matter more than the brand name.
Starting Out: What to Expect
Most women start with the lowest dose possible. For estrogen, that’s often 0.5mg of estradiol or 0.3mg of conjugated estrogens. For progestogen, 100mg of micronized progesterone daily or 2.5mg of MPA.It takes 3-6 months to find your sweet spot. You might have breakthrough bleeding in the first few months-that’s normal. If it lasts longer than six months, your dose or delivery method might need adjusting.
Transdermal gels require daily application and no skin-to-skin contact for an hour after. Patches need to be changed twice a week and rotated to avoid skin irritation. IUS insertion requires a quick office visit. Each method has a learning curve.
Long-Term Use and Reassessment
There’s no fixed end date for HRT. The goal isn’t to take it forever-it’s to take it only as long as you need it.The North American Menopause Society now recommends annual reviews after 3-5 years. Ask yourself: Are your hot flashes gone? Is your sleep better? Do you still need it? If the answer is no, it’s time to taper down.
For women who start HRT under 60 or within 10 years of menopause, the benefits still outweigh the risks-for the right person, for the right time. But if you’re 70 and still on it because “you’ve always taken it,” that’s not a plan. That’s inertia.
The Future of Hormone Therapy
New options are coming. In 2023, the FDA approved a new transdermal patch combining estradiol and progesterone-early data suggests it may lower breast cancer risk even further than current options.Researchers are also testing tissue-selective estrogen complexes (TSECs) and selective progesterone receptor modulators (SPRMs). These aim to give you the benefits of hormones without the cancer risks. They’re still in trials, but they’re the next big thing.
For now, stick with what works: low-dose, generic, transdermal, and tailored to your body. Don’t let fear stop you. Don’t let convenience trap you. Hormone therapy isn’t a one-size-fits-all solution. It’s a personalized tool-and used right, it can give you back years of quality life.


Paul Ong
Just took the patch last month and my hot flashes are gone like magic
no more midnight sweat sessions
Richard Thomas
There’s something deeply human about how we’ve come to treat hormonal shifts as problems to be fixed rather than natural transitions we’ve spent centuries misunderstanding. We’ve built entire industries around masking biology instead of listening to it. The fact that we’re now prioritizing transdermal delivery over oral pills isn’t just medical progress-it’s a quiet reclamation of bodily autonomy. And yet, most women still feel pressured to take the cheapest, most convenient option, even when it’s riskier. The real question isn’t which hormone to take-it’s whether our healthcare system is willing to support the kind of personalized care that actually respects the complexity of the female body. We’ve got the science. We just haven’t yet built the culture to match it.
Todd Nickel
Interesting that the WHI data shows a 21% reduction in type 2 diabetes with continuous combined HRT. I’ve seen that number cited before, but rarely connected to the delivery method. Transdermal estrogen’s hepatic avoidance likely plays a role here-less first-pass metabolism means less insulin resistance triggered by liver stress. Also worth noting: micronized progesterone’s lower breast cancer risk isn’t just about the molecule-it’s about how it interacts with estrogen receptor beta in breast tissue versus synthetic progestins binding to alpha receptors. That’s not just semantics; it’s why some women on MPA develop dense mammograms while those on Prometrium don’t.
Bryan Anderson
Thank you for this thoughtful breakdown. I’ve been on low-dose estradiol gel for 18 months now and the difference in sleep and mood has been profound. I appreciate how you emphasized that HRT isn’t for prevention-it’s for symptom relief. Too many people think it’s a longevity hack, and that sets unrealistic expectations. Also, the point about annual reassessment is critical. My doctor didn’t bring it up until year three-I had to ask. We need more of these conversations to be proactive, not reactive.
sharad vyas
From India, we don’t have easy access to transdermal options. Most women here get oral pills because they’re cheaper and available without prescription. But I’ve seen friends on MPA develop severe mood swings-switched them to micronized progesterone and it was night and day. The science is clear, but access isn’t. We need global equity in HRT options, not just US-centric advice.
Alex Warden
They want you on patches so they can sell you more stuff
Big Pharma doesn’t care if you feel better
they care if you stay on it forever
Lee M
Let’s be real-this whole HRT industry is built on fear. Fear of aging, fear of sweating, fear of being ‘unfeminine’ because your body changed. But what if the real solution isn’t hormones at all? What if it’s learning to live with the change instead of medicating it away? We’ve turned menopause into a disease because capitalism needs a market. The truth? Most women don’t need pills. They need community, rest, and permission to be tired.
Stephen Gikuma
They’re pushing transdermal because it’s easier to track you. GPS patches. Biometric monitoring. Next thing you know, your hormone levels are being fed to insurance companies. This isn’t healthcare-it’s surveillance with estrogen.
Andy Heinlein
Just got my first Mirena and holy crap it’s been a game changer
no more monthly drama and my skin cleared up
also the doc said I can use it with a patch
best combo i’ve found so far 😎
Dusty Weeks
Y’all are overthinking this. Just take the Walmart $10 pill and chill 🤷♂️💊
LIZETH DE PACHECO
I’m a nurse and I’ve seen too many women quit HRT because they were scared of breast cancer. But the numbers? Less than 1 in 1,000 per year. That’s less risk than driving to the grocery store. If you’re under 60 and your symptoms are wrecking your life, please don’t let fear silence you. Talk to your doctor. Try the lowest dose. Give it time. You deserve to feel like yourself again.
Paul Ong
That patch I’m on? I forgot to change it last week
still felt fine
maybe I’m just lucky
Matthew Hekmatniaz
Shoutout to the commenters who mentioned micronized progesterone. I switched from MPA after 3 years and my anxiety dropped off a cliff. It’s not just about cancer risk-it’s about brain chemistry. Progesterone is a GABA modulator. Synthetic progestins? Not so much. If you’re feeling ‘off’ on HRT, ask your doc about Prometrium. It’s not glamorous, but it’s gentle.
Bobby Collins
They’re putting estrogen in the water. That’s why more women are getting cancer now. You think it’s coincidence? Look at the numbers. The government doesn’t want you to know this.
Liam George
Let’s not ignore the epigenetic implications of exogenous hormone exposure during the critical window of postmenopausal transition. The methylation patterns of BRCA1 and ERα promoters are dynamically responsive to ligand binding, and chronic synthetic progestin exposure may induce transcriptional silencing via HDAC recruitment. While micronized progesterone appears to preserve chromatin accessibility, the long-term transcriptomic consequences remain underexplored in population-level cohorts. The current clinical paradigm prioritizes symptom suppression over molecular fidelity-a dangerous reductionism.